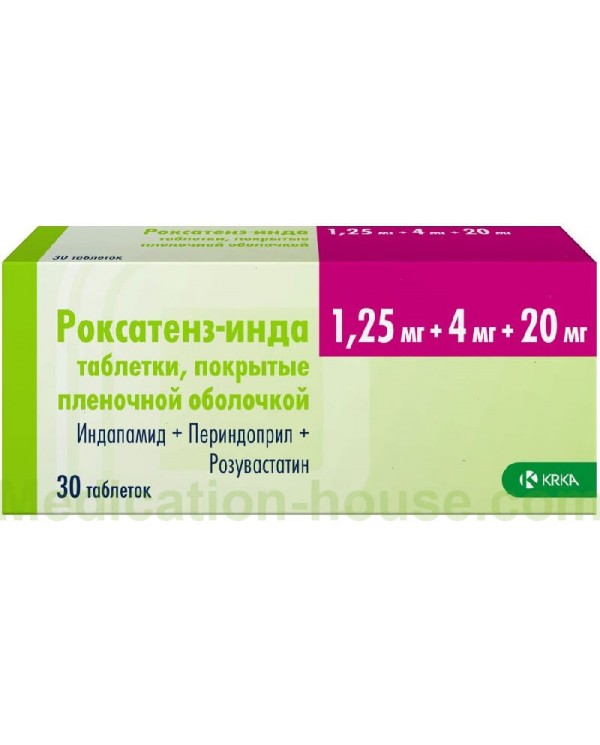
Roxatenz-Inda instruction
You can buy Roxatenz-Inda here
Pharmachologic effect
Roxatenz-Inda containing perindopril, an ACE inhibitor, indapamide, a thiazide-like diuretic, and rosuvastatin, a selective, competitive inhibitor of HMG-CoA reductase (statin).
Indapamide
Indapamide is a sulfonamide derivative, with pharmacological properties similar to thiazide diuretics. Indapamide inhibits the reabsorption of sodium ions in the cortical segment of Henle's loop, which leads to an increase in the excretion of sodium ions, chlorine and, to a lesser extent, potassium and magnesium ions by the kidneys, thereby increasing diuresis and reducing blood pressure.
Perindopril
Perindopril is an inhibitor of the enzyme that converts angiotensin I to angiotensin II, a vasoconstrictor; in addition, ACE stimulates the secretion of aldosterone and the destruction of bradykinin, which has a vasodilating effect, to an inactive heptapeptide.
As a result, perindopril: reduces the secretion of aldosterone; according to the principle of negative feedback, increases the activity of renin in the blood plasma; with prolonged use, it reduces OPSS, which is mainly due to the effect on the vessels in the muscles and kidneys.
These effects are not accompanied by the retention of sodium ions or fluid, or the development of reflex tachycardia.
Perindopril has an antihypertensive effect in patients with both low and normal renin activity in blood plasma.
Perindopril acts through its main active metabolite, perindoprilat. Its other metabolites are inactive.
The action of perindopril leads to: varicose veins (decreased preload on the heart) due to changes in prostaglandin metabolism; decrease in OPSS (decrease in afterload on the heart).
The study of hemodynamic parameters in patients with chronic heart failure (CHF) revealed: a decrease in filling pressure in the left and right ventricles of the heart; decrease in OPSS; increased cardiac output and increased cardiac index; increased muscle peripheral blood flow.
As a result, the results of the exercise test are significantly improved.
Rosuvastatin
Rosuvastatin is a selective, competitive inhibitor of HMG-CoA reductase, an enzyme that converts 3-hydroxy-3-methylglutaryl coenzyme A to mevalonic acid, a cholesterol precursor.
Rosuvastatin increases the number of "hepatic" LDL receptors on the cell surface, increasing the uptake and catabolism of LDL, which in turn leads to inhibition of VLDL synthesis, thereby reducing the total amount of LDL and VLDL.
Indications for Roxatenz-Inda
Treatment of arterial hypertension and concomitant dyslipidemia: primary hypercholesterolemia (type IIa according to Fredrickson's classification, including familial heterozygous hypercholesterolemia), mixed hypercholesterolemia (type IIb according to Fredrickson's classification) or familial homozygous hypercholesterolemia.
Method of application, course and dosage
Inside, 1 single dose 1 time per day. The dose should be determined by the doses of monopreparations that are part of the fixed combination at the time of transition to treatment with this drug.
Drug interactions
For perindopril and indapamide
Simultaneous use is not recommended
Lithium preparations: with the simultaneous use of lithium preparations and ACE inhibitors, cases of a reversible increase in the content of lithium in the blood plasma and associated toxic effects have been reported. The simultaneous use of thiazide diuretics can further increase the lithium content in the blood plasma and increase the risk of its toxic effect while taking an ACE inhibitor. The simultaneous use of a combination of perindopril and indapamide with lithium preparations is not recommended. If necessary, simultaneous use must carefully monitor the content of lithium in blood plasma.
MTOR inhibitors (eg, sirolimus, everolimus, temsirolimus): when used concomitantly with mTOR inhibitors, therapy may be associated with an increased risk of angioedema.
Simultaneous use of drugs requiring special attention
Baclofen: Possible increased antihypertensive action. It is necessary to control blood pressure, renal function and, if necessary, adjust the dose of antihypertensive drugs.
NSAIDs, including high doses of acetylsalicylic acid (≥3 g / day): the simultaneous use of ACE inhibitors and NSAIDs (including acetylsalicylic acid in doses that have anti-inflammatory effects, COX-2 inhibitors and non-selective NSAIDs) can lead to a decrease in the antihypertensive effect ACE inhibitors, increases the risk of developing renal dysfunction, up to the development of acute renal failure, increases serum potassium, especially in patients with initially reduced renal function.
Caution should be exercised when using this combination, especially in elderly patients. Before starting treatment, patients need to compensate for fluid loss, as well as regularly monitor kidney function both at the beginning of therapy and during treatment.
Simultaneous use requiring attention
Tricyclic antidepressants, antipsychotics (antipsychotics): drugs in these classes increase the antihypertensive effect and increase the risk of orthostatic hypotension (additive effect).
GCS, tetracosactide: a decrease in the antihypertensive effect (retention of fluid and sodium ions as a result of the action of GCS).
Other antihypertensive drugs: an increase in the antihypertensive effect is possible.
For indapamide
Simultaneous application requiring special attention
Drugs that can cause polymorphic ventricular tachycardia of the "pirouette" type: since there is a risk of hypokalemia, indapamide should be used with caution simultaneously with drugs that can cause polymorphic ventricular tachycardia of the "pirouette" type, such as class IA antiarrhythmics (quinidine, hydroquinidine, disopyramide) and class III (amiodarone, dofetilide, ibutilide, bretylium tosylate, sotalol), some antipsychotics (chlorpromazine, cyamemazine, levomepromazine, thioridazine, trifluoperazine), benzamides (amisulpride, sulpridylamide, thirophenol ), other antipsychotics (pimozide), other drugs such as bepridil, cisapride, diphemanil methyl sulfate, erythromycin for i.v. use, halofantrine, mizolastine, moxifloxacin, pentamidine, sparfloxacin, vincamine for i / v use, methadone, astemisine. It is necessary to control the content of potassium in the blood serum in order to avoid hypokalemia, with the development of which it is necessary to carry out its correction, to control the QT interval on the ECG.
Medicines that can cause hypokalemia: amphotericin B when administered intravenously, gluco- and mineralocorticoids (for systemic administration), tetracosactide, laxatives that stimulate intestinal motility: an increased risk of hypokalemia (additive effect). It is necessary to control the content of potassium in the blood plasma, if necessary, to correct it. Particular attention should be paid to patients simultaneously receiving cardiac glycosides. Use laxatives that do not stimulate intestinal motility.
Cardiac glycosides: hypokalemia enhances the toxic effects of cardiac glycosides. With the simultaneous use of indapamide and cardiac glycosides, the content of potassium in the blood plasma, ECG indicators should be monitored and, if necessary, the therapy should be adjusted.
Simultaneous use requiring attention
Metformin: functional renal failure while taking diuretics, especially loop diuretics, when used simultaneously with metformin, increases the risk of lactic acidosis. Do not use metformin if the plasma creatinine concentration exceeds 15 mg / L (135 μmol / L) in men and 12 mg / L (110 μmol / L) in women.
Iodine-containing contrast agents: in patients with hypovolemia during therapy with diuretics, there is an increased risk of developing acute renal failure, especially when using contrast agents containing high doses of iodine. Before using iodine-containing contrast media, the BCC should be replenished.
Preparations containing calcium salts: with simultaneous use, hypercalcemia may develop due to a decrease in calcium excretion by the kidneys.
Cyclosporine: it is possible to increase the concentration of creatinine in the blood plasma without changing the concentration of cyclosporine in the blood plasma, even in the absence of a pronounced loss of sodium ions and dehydration.
For perindopril
Data from clinical trials have shown that double blockade of the RAAS as a result of the simultaneous administration of ACE inhibitors, ARA II or aliskiren leads to an increase in the incidence of such adverse events as arterial hypotension, hyperkalemia and impaired renal function (including ARF), compared with the use of only one drug acting on the RAAS.
The simultaneous use of ACE inhibitors with ARA II in patients with diabetic nephropathy is contraindicated and not recommended in other patients.
Simultaneous use is contraindicated
Aliskiren and drugs containing aliskiren: the simultaneous use of ACE inhibitors with aliskiren or drugs containing aliskiren in patients with diabetes and / or moderate or severe renal impairment (GFR less than 60 ml / min / 1.73 m2) is contraindicated and not recommended in others patients.
Neutral endopeptidase inhibitors: An increased risk of angioedema has been reported with concomitant use of ACE inhibitors and racecadotril (an enkephalinase inhibitor).
With the simultaneous use of ACE inhibitors with drugs containing sacubitril (neprilisin inhibitor), the risk of developing angioedema increases, and therefore the simultaneous use of these drugs is contraindicated. ACE inhibitors should be prescribed no earlier than 36 hours after discontinuation of drugs containing sacubitrile. The appointment of preparations containing sacubitril is contraindicated in patients receiving ACE inhibitors, as well as within 36 hours after discontinuation of ACE inhibitors.
Extracorporeal treatments: Extracorporeal treatments using certain high-flow membranes with a negatively charged surface (eg, polyacrylonitrile), such as hemodialysis or hemofiltration, and LDL apheresis using dextran sulfate are contraindicated due to the increased risk of severe anaphylactoid reactions. If the patient requires extracorporeal therapies, consider using a different type of dialysis membrane or a different class of antihypertensive drugs.
Simultaneous use is not recommended
Potassium-sparing diuretics (amiloride, spironolactone, eplerenone, triamterene, both in monotherapy and in combination therapy) and potassium supplements: ACE inhibitors reduce kidney potassium loss caused by a diuretic. With simultaneous use with ACE inhibitors, it is possible to increase the content of potassium in the blood serum, up to a lethal outcome. If the simultaneous use of an ACE inhibitor and the above drugs is necessary (in the case of confirmed hypokalemia), care should be taken and regular monitoring of plasma potassium and ECG parameters should be carried out.
Estramustine: Concomitant use may increase the risk of side effects such as angioedema.
Simultaneous application requiring special attention
Oral hypoglycemic agents (sulfonylurea derivatives) and insulin: The following effects are described for captopril and enalapril. The use of ACE inhibitors can enhance the hypoglycemic effect of sulfonylurea and insulin derivatives in patients with diabetes. The development of hypoglycemia is very rare (due to an increase in glucose tolerance and a decrease in insulin requirements).
Simultaneous use requiring attention
Antihypertensives and vasodilators: the simultaneous use of these drugs can enhance the antihypertensive effect of perindopril. With simultaneous administration with nitroglycerin, other nitrates or other vasodilators, an additional decrease in blood pressure is possible.
Allopurinol, cytostatic and immunosuppressive agents, GCS (with systemic use) and procainamide: simultaneous use with ACE inhibitors may increase the risk of leukopenia.
Preparations for general anesthesia: the simultaneous use of ACE inhibitors and agents for general anesthesia can lead to an increase in the antihypertensive effect.
Diuretics (thiazide and "loop"): the use of diuretics in high doses can lead to hypovolemia (due to a decrease in BCC), and the addition of perindopril to therapy - to a pronounced decrease in blood pressure.
Gliptins (linagliptin, saxagliptin, sitagliptin, vildagliptin): when used simultaneously with ACE inhibitors, the risk of angioedema increases due to suppression of DPP-4 activity by gliptin.
Sympathomimetics: May weaken the antihypertensive effect of ACE.
Gold preparations: with the simultaneous use of ACE inhibitors, including perindopril, and intravenous administration of a gold preparation (sodium aurothiomalate), a symptom complex is described, including flushing of the skin of the face, nausea, vomiting and a pronounced decrease in blood pressure.
Co-trimoxazole (sulfamethoxazole + trimethoprim): concomitant use with ACE inhibitors may increase the risk of hyperkalemia.
Tissue plasminogen activators: observational studies have shown an increased incidence of angioedema in patients taking ACE inhibitors after using alteplase for thrombolytic therapy of ischemic stroke.
For rosuvastatin
Effect of other drugs on rosuvastatin
Inhibitors of transport proteins: rosuvastatin is a substrate for several transport proteins, in particular OATP1B1 and BCRP. The simultaneous use of drugs that are inhibitors of these transport proteins may be accompanied by an increase in the concentration of rosuvastatin in the blood plasma and an increased risk of myopathy.
Cyclosporin: with the simultaneous use of rosuvastatin and cyclosporin, the AUC of rosuvastatin is on average 7 times higher than that observed in healthy volunteers. Concomitant use with rosuvastatin does not affect the plasma concentration of cyclosporine. The use of rosuvastatin is contraindicated in patients taking cyclosporine. Concomitant use with rosuvastatin does not affect the plasma concentration of cyclosporine.
Protease inhibitors: Despite the fact that the exact mechanism of interaction has not been established, the simultaneous use of protease inhibitors can significantly increase the exposure of rosuvastatin. The simultaneous use of 10 mg of rosuvastatin and a combination of two protease inhibitors (300 mg of atazanavir / 100 mg of ritonavir) in healthy volunteers is accompanied by an increase in the equilibrium AUC (0-24 hours) and Cmax of rosuvastatin by 3 and 7 times, respectively. The simultaneous use of rosuvastatin and some combinations of protease inhibitors is possible only after careful adjustment of the dose of rosuvastatin based on the expected increase in its exposure.
Gemfibrozil and other lipid-lowering agents: the simultaneous use of rosuvastatin and gemfibrozil leads to a 2-fold increase in Cmax and AUC of rosuvastatin in blood plasma. Based on specific interaction data, no pharmacokinetically significant interaction with fenofibrate is expected, but pharmacodynamic interaction is possible. Gemfibrozil, fenofibrate, other fibrates, as well as nicotinic acid in lipid-lowering doses (more than 1 g / day) increased the risk of myopathy when used simultaneously with HmG-CoA reductase inhibitors, possibly due to the fact that they can cause myopathy when used in monotherapy. In these patients, therapy should begin with a dose of 5 mg. The simultaneous use of fibrates and rosuvastatin in a daily dose of 30 mg and 40 mg is contraindicated.
Ezetimibe: the simultaneous use of rosuvastatin at a dose of 10 mg and ezetimibe at a dose of 10 mg was accompanied by an increase in the AUC of rosuvastatin in patients with hypercholesterolemia by 1-2 times. A pharmacodynamic interaction between rosuvastatin and ezetimibe, which is manifested by an increase in the risk of developing adverse reactions, cannot be ruled out.
Antacids: the simultaneous use of rosuvastatin and antacids containing aluminum and magnesium hydroxide leads to a decrease in the plasma concentration of rosuvastatin by about 50%. This effect is less pronounced if antacids are used 2 hours after taking rosuvastatin. The clinical significance of this interaction has not been studied.
Erythromycin: the simultaneous use of rosuvastatin and erythromycin leads to a decrease in the AUC (0-t) of rosuvastatin by 20% and its Cmax by 30%. This interaction can occur as a result of increased intestinal motility caused by the use of erythromycin.
Isozymes of the cytochrome P450 system: the results of studies carried out in vivo and in vitro have shown that rosuvastatin is neither an inhibitor nor an inducer of isoenzymes of the cytochrome P450 system. In addition, rosuvastatin is a weak substrate for this isoenzyme system. Therefore, the interaction of rosuvastatin with other drugs at the metabolic level with the participation of isoenzymes of the cytochrome P450 system is not expected.
There was no clinically significant interaction between rosuvastatin and fluconazole (an inhibitor of CYP2C9 and CYP3A4 isoenzymes) and ketoconazole (an inhibitor of CYP2A6 and CYP3A4 isoenzymes).
Effect of rosuvastatin use on other drugs
Vitamin K antagonists: as with other HMG-CoA reductase inhibitors, initiation of rosuvastatin therapy or an increase in its dose in patients taking concomitantly vitamin K antagonists (for example, warfarin or other coumarin anticoagulants) may lead to an increase in INR. Cancellation of rosuvastatin or a decrease in its dose may lead to a decrease in INR. In such cases, INR control is recommended.
Oral contraceptives / HRT
The simultaneous use of rosuvastatin and oral contraceptives increases the AUC of ethinyl estradiol and norgestrel by 26% and 34%, respectively. Such an increase in plasma concentration should be taken into account when selecting a dose of hormonal contraceptives.
Pharmacokinetic data on the simultaneous use of rosuvastatin and HRT are absent, therefore, a similar effect cannot be excluded when using this combination. However, this combination was widely used during clinical trials and was well tolerated by patients.
Other medicines
Digoxin: No clinically significant interaction of rosuvastatin with digoxin is expected.
Fusidic acid: the risk of developing myopathy, including rhabdomyolysis, may be increased with the simultaneous use of systemic fusidic acid and statins. The mechanism of this interaction (pharmacodynamic, pharmacokinetic, or both) has not been established. There have been reports of rhabdomyolysis (including fatalities) in patients receiving this combination.
If necessary, the simultaneous use should stop taking rosuvastatin for the period of therapy with fusidic acid.
Application during pregnancy and lactation
Use during pregnancy and lactation (breastfeeding) is contraindicated.
Side effect of Roxatenz-Inda
Infectious and parasitic diseases: rhinitis.
Blood and lymphatic system disorders: eosinophilia, agranulocytosis, aplastic anemia, pancytopenia, leukopenia, neutropenia, hemolytic anemia, thrombocytopenia.
From the immune system: hypersensitivity reactions (especially reactions from the skin, in patients prone to allergic and asthmatic reactions).
From the endocrine system: type 2 diabetes mellitus.
From the side of metabolism and nutrition: hypoglycemia, hyperkalemia, more often transient, hyponatremia, hypercalcemia, a decrease in potassium with the development of hypokalemia, especially important for patients from high-risk groups.
From the side of the psyche: mood disturbance, sleep disorder, confusion, depression.
From the nervous system: dizziness, headache, paresthesia, dysgeusia, drowsiness, fainting, peripheral neuropathy, polyneuropathy, memory loss, stroke, possibly due to an excessive decrease in blood pressure in high-risk patients, hepatic encephalopathy may develop in case of liver failure.
From the side of the organ of vision: visual impairment, myopia, blurred vision.
On the part of the organ of hearing and labyrinth disorders: vertigo, tinnitus.
From the heart: palpitations, tachycardia, angina pectoris, arrhythmias (including bradycardia, ventricular tachycardia and atrial fibrillation), myocardial infarction, possibly due to an excessive decrease in blood pressure in high-risk patients.
From the side of the vessels: arterial hypotension (and the effects associated with arterial hypotension), vasculitis, Raynaud's syndrome.
From the respiratory system, chest and mediastinal organs: cough, shortness of breath, bronchospasm, eosinophilic pneumonia.
From the gastrointestinal tract: abdominal pain, constipation, diarrhea, dyspepsia, nausea, vomiting, dryness of the oral mucosa, pancreatitis.
From the liver and biliary tract: hepatitis, liver dysfunction, jaundice.
On the part of the skin and subcutaneous tissues: skin itching, skin rash, maculopapular rash, urticaria, angioedema of the face, lips, extremities, mucous membrane of the tongue, vocal folds and / or larynx, purpura, increased sweating, photosensitivity reactions, pemphigoid, psoriasis aggravation , erythema multiforme, toxic epidermal necrolysis, Stevens-Johnson syndrome.
From the musculoskeletal system and connective tissue: muscle spasms, possible exacerbation of an existing acute disseminated lupus erythematosus, arthralgia, myalgia, myopathy (including myositis), rhabdomyolysis, lupus-like syndrome, muscle rupture, tendon damage, immune-mediated necrotizing myopathy.
From the kidneys and urinary tract: renal failure, acute renal failure, hematuria.
From the genitals and mammary gland: erectile dysfunction, gynecomastia.
Systemic reactions: asthenia, back pain, malaise, peripheral edema, pyrexia, fatigue.
Laboratory and instrumental data: an increase in the concentration of urea, uric acid, creatinine, bilirubin in the blood plasma, an increase in the activity of "liver" enzymes, a decrease in hemoglobin and a decrease in hematocrit, an increase in the concentration of glucose in the blood plasma, an extension of the QT interval on the electrocardiogram.
Contraindications for use of Roxatenz-Inda
A history of angioedema (Quincke's edema) associated with the use of ACE inhibitors; hereditary / idiopathic angioedema; severe renal failure (CC less than 30 ml / min); severe hepatic impairment (including with hepatic encephalopathy); liver disease in the active phase (including a persistent increase in the activity of hepatic transaminases and an increase in the activity of hepatic transaminases in the blood serum by more than 3 times compared with VGN); myopathy; patients prone to the development of myotoxic complications; hypokalemia; simultaneous use with drugs that can cause polymorphic ventricular arrhythmias of the "pirouette" type; concomitant use of cyclosporine; simultaneous use with aliskiren or preparations containing aliskiren in patients with diabetes mellitus and / or moderate or severe renal impairment (GFR less than 60 ml / min / 1.73 m2 of body surface area); simultaneous use with angiotensin II receptor antagonists in patients with diabetic nephropathy; simultaneous use with inhibitors of neutral endopeptidase (for example, with preparations containing sacubitrile) due to the high risk of developing angioedema; extracorporeal treatments using certain membranes with a negatively charged surface; severe bilateral renal artery stenosis or renal artery stenosis of a single functioning kidney; use in women of childbearing age who do not use adequate methods of contraception; pregnancy, breastfeeding period; age up to 18 years (efficacy and safety have not been established); due to the lack of sufficient clinical experience, it should not be used in patients on hemodialysis, as well as in patients with untreated heart failure in the stage of decompensation.
Carefully
Systemic connective tissue diseases (SLE, scleroderma), immunosuppressive therapy (risk of neutropenia, agranulocytosis), inhibition of bone marrow hematopoiesis, decreased BCC (intake of diuretics, diet with salt restriction, vomiting, diarrhea), ischemic heart disease, cerebrovascular and liver dysfunction kidney, renovascular hypertension, diabetes mellitus, CHF (NYHA functional class IV), hyperuricemia (especially accompanied by gout and urate nephrolithiasis), blood pressure lability, use in elderly patients, blacks, athletes (a positive reaction is possible with doping control) , carrying out hemodialysis using high-flow polyacrylonitrile membranes (for example, AN69), before the LDL apheresis procedure, concurrent desensitizing therapy with allergens (for example, Hymenoptera venom), condition after kidney transplantation, aortic and / or mitral valve stenosis, hypertrophic obstructive i cardiomyopathy, bilateral stenosis of the renal arteries, stenosis of the artery of a single kidney, simultaneous use with lithium, gold, NSAIDs, baclofen, corticosteroids, drugs that can cause polymorphic ventricular tachycardia of the "pirouette" type, the presence of a risk of myopathy / rhabdomyolysis, renal hypothyroidism a history of hereditary muscle disease (including family history) and a previous history of muscle toxicity with the use of other HMG-CoA reductase inhibitors or fibrates; excessive alcohol consumption, conditions in which an increase in the plasma concentration of rosuvastatin was noted, race (Mongoloid race - Japanese and Chinese), simultaneous use with fibrates, a history of liver disease, sepsis, arterial hypotension, major surgical interventions, trauma, severe metabolic, endocrine or electrolyte disturbances or uncontrolled convulsions, concomitant use with ezetimibe.
Special instructions for Roxatenz-Inda
Impaired renal function
In patients with severe renal impairment (CC <30 ml / min), use is contraindicated.
In patients with CC <60 ml / min, an individual selection of doses of individual active components that make up Roxatenz-Inda is recommended.
Elderly patients
Before starting to take Roxatenz-Inda, it is necessary to assess the functional activity of the kidneys and the potassium content in the blood plasma. At the beginning of therapy, the dose is selected, taking into account the degree of decrease in blood pressure, especially in the case of a decrease in BCC and loss of electrolytes, which avoids a sharp decrease in blood pressure.
Diabetes
In patients with diabetes mellitus receiving oral hypoglycemic agents or insulin, during the first month of treatment with an ACE inhibitor, regular monitoring of the plasma glucose concentration is necessary.
It is necessary to monitor the concentration of glucose in the blood in patients with diabetes, especially with low potassium in the blood plasma.
Perindopril / Indapamide
Arterial hypotension and imbalance in water and electrolyte balance
Patients with hyponatremia (especially with renal artery stenosis, including bilateral) have a risk of sudden development of arterial hypotension. Therefore, attention should be paid to possible symptoms of dehydration and a decrease in the content of electrolytes in the blood plasma, for example, after diarrhea or vomiting. Such patients need regular monitoring of blood plasma electrolytes. With severe arterial hypotension, intravenous administration of 0.9% sodium chloride solution may be required.
Transient arterial hypotension is not a contraindication for continued therapy. After the restoration of BCC and blood pressure, therapy can be resumed using low doses of a combination of perindopril and indapamide, or only one of the drugs.
Renovascular hypertension
In patients with bilateral renal artery stenosis or renal artery stenosis of a single functioning kidney during therapy with ACE inhibitors, the risk of arterial hypotension and renal failure increases. Taking diuretics can be an additional risk factor. Deterioration of renal function can be observed even with a slight change in the concentration of creatinine in the blood plasma, even in patients with unilateral renal artery stenosis.
The treatment of renovascular hypertension is revascularization. Nevertheless, the use of ACE inhibitors can be effective in patients with renovascular hypertension, both awaiting surgery and when it is not possible to perform it.
In patients with diagnosed or suspected renal artery stenosis, treatment with indapamide / perindopril should be initiated in a hospital setting.
The risk of arterial hypotension and / or renal failure (in patients with CHF, impaired water and electrolyte balance, etc.)
In some pathological conditions, there may be a significant activation of the RAAS, especially with severe hypovolemia and a decrease in the content of blood plasma electrolytes (against the background of a salt-free diet or long-term use of diuretics), in patients with initially low blood pressure, renal artery stenosis, CHF or liver cirrhosis with edema and ascites ...
The use of ACE inhibitors causes a blockade of the RAAS and, therefore, may be accompanied by a sharp decrease in blood pressure and / or an increase in plasma creatinine concentration, indicating the development of functional renal failure. These phenomena are more often observed when taking the first dose of Roxatenz-Inda or during the first two weeks of therapy. Sometimes these conditions develop sharply at other times of therapy. In such cases, when resuming therapy, it is recommended to use a combination of perindopril and indapamide at a lower dose and then gradually increase the dose.
Heart failure / severe heart failure
In patients with CHF (NYHA functional class IV) and patients with type 1 diabetes (the risk of a spontaneous increase in the content of potassium ions), treatment should begin with lower doses of the combination of perindopril and indapamide and under close medical supervision.
Patients with hypertension and ischemic heart disease should not stop taking beta-blockers, the combination of perindopril and indapamide should be used in conjunction with beta-blockers.
Liver failure
In rare cases, cholestatic jaundice occurs while taking ACE inhibitors. With the progression of this syndrome, fulminant necrosis of the liver develops, sometimes with a fatal outcome. The mechanism for the development of this syndrome is unclear. With a significant increase in the activity of "liver" enzymes or the appearance of jaundice while taking ACE inhibitors, you should stop taking Roxatenz-Inda and continue monitoring the patient.
In the presence of liver dysfunction, taking thiazide and thiazide-like diuretics can lead to the development of hepatic encephalopathy. In this case, you should immediately stop taking Roxatenz-Inda.
Indapamide
Photosensitivity
While taking thiazide and thiazide-like diuretics, cases of photosensitivity reactions have been reported. If a photosensitivity reaction develops, treatment should be discontinued. If it is necessary to continue diuretic therapy, it is recommended to protect the skin from exposure to sunlight or artificial ultraviolet rays.
Plasma sodium content
Before starting treatment, it is necessary to determine the sodium content in the blood plasma. While taking this combination, this indicator should be regularly monitored. At the initial stage of therapy, a decrease in the sodium content in the blood plasma may be asymptomatic, therefore, regular laboratory monitoring is necessary. Elderly patients and patients with liver cirrhosis are shown more frequent monitoring of the sodium content in the blood plasma.
Any diuretic drug can cause hyponatremia, sometimes leading to extremely serious consequences.
Hyponatremia combined with hypovolemia can cause dehydration and orthostatic hypotension.
A concomitant decrease in the content of chlorine in the blood plasma can lead to secondary compensatory metabolic alkalosis (the frequency of development and the severity of this effect are insignificant).
Plasma potassium
Therapy with thiazide and thiazide-like diuretics is associated with the risk of hypokalemia. It is necessary to avoid hypokalemia (less than 3.4 mmol / L) in the following categories of patients from high risk groups: elderly patients, malnourished patients (both receiving and not receiving combined drug therapy), patients with liver cirrhosis, including edema and ascites , patients with ischemic heart disease, CHF. In these patients, hypokalemia increases the toxic effects of cardiac glycosides and increases the risk of arrhythmias.
The combined use of perindopril and indapamide does not prevent the development of hypokalemia, especially in patients with diabetes mellitus or renal failure. As in the case of the use of other antihypertensive drugs in combination with a diuretic, regular monitoring of the potassium content in the blood plasma is necessary.
Prolongation of the QT interval
The increased risk group also includes patients with an increased QT interval, and it does not matter if this increase is caused by congenital causes or the action of drugs. Hypokalemia, like bradycardia, contributes to the development of severe cardiac arrhythmias, especially polymorphic ventricular tachycardia of the "pirouette" type, which can be fatal.
In all the cases described above, regular monitoring of the initiation of therapy is necessary.
If hypokalemia is detected, appropriate treatment should be prescribed.
Plasma calcium
Thiazide and thiazide-like diuretics reduce the excretion of calcium by the kidneys, which can cause a slight temporary increase in plasma calcium. Severe hypercalcemia may be associated with previously undiagnosed hyperparathyroidism. In such cases, it is necessary to conduct a study of the function of the parathyroid glands, having previously canceled the intake of diuretics.
Diuretics and kidney function
Thiazide and thiazide-like diuretics are fully effective only in patients with normal or slightly impaired renal function (plasma creatinine concentration in adult patients is below 25 mg / L or 220 μmol / L). In elderly patients, the normative indicator for the concentration of creatinine in the blood plasma should be adjusted for age, weight and sex, in accordance with the Cockcroft formula:
CC = (140 - age) x weight / 0.814 x plasma creatinine concentration,
where: age is indicated in years, weight - in kg, creatinine concentration - in μmol / l.
For women, this formula should be adjusted by multiplying the result by a factor of 0.85.
At the beginning of diuretic treatment in patients due to hypovolemia and hyponatremia, there may be a temporary decrease in GFR and an increase in the concentration of urea and creatinine in the blood plasma. This transient functional renal failure is not dangerous in patients with unchanged renal function, but in patients with renal failure, its severity may increase.
Uric acid
In patients with an increased concentration of uric acid in the blood plasma during therapy, the incidence of gout attacks may increase.
Athletes
Indapamide can give a positive reaction during doping control.
Acute myopia and secondary acute angle-closure glaucoma
Sulfonamides and their derivatives can cause an idiosyncratic reaction leading to the development of acute transient myopia and an acute attack of angle-closure glaucoma. If left untreated, an acute attack of angle-closure glaucoma can lead to permanent loss of vision. First of all, it is necessary, as soon as possible, to stop taking Roxatenz-Inda. If intraocular pressure remains uncontrolled, urgent medical treatment or surgery may be required. Risk factors for the development of an acute attack of angle-closure glaucoma are allergic reactions to sulfonamide derivatives and penicillins in history.
Perindopril
Double blockade of RAAS
There is evidence of an increased risk of arterial hypotension, hyperkalemia and impaired renal function (including acute renal failure) with the simultaneous use of ACE inhibitors with ARA II or aliskiren. Therefore, double blockade of RAAS by combining an ACE inhibitor with ARA II or aliskiren is not recommended. If double blockade is necessary, then this should be performed under the strict supervision of a specialist with regular monitoring of renal function, plasma potassium and blood pressure. ACE inhibitors should not be used concomitantly with ARA II in patients with diabetic nephropathy.
Neutropenia / Agranulocytosis / Thrombocytopenia / Anemia
While taking ACE inhibitors, neutropenia / agranulocytosis, thrombocytopenia and anemia may occur. In patients with normal renal function in the absence of other risk factors, neutropenia rarely develops. After the abolition of the ACE inhibitor, neutropenia and agranulocytosis go away on their own. Perindopril should be used with extreme caution in patients with systemic connective tissue diseases (including systemic lupus erythematosus, scleroderma) during therapy with immunosuppressants, allopurinol or procainamide, especially in patients with impairment; kidney function.
Some patients developed severe infections, in some cases resistant to intensive antibiotic therapy. When using perindopril in such patients, it is recommended to periodically monitor the number of leukocytes in the blood plasma. If any symptoms of infectious diseases appear (eg, sore throat, fever), patients should consult a doctor.
Hypersensitivity / angioedema
While taking ACE inhibitors, including perindopril, in rare cases, there may be the development of angioedema of the face, limbs, lips, tongue, vocal folds and / or larynx. This can happen at any time during therapy. If symptoms appear, you should immediately stop taking Roxatenz-Inda and continue monitoring the patient until symptoms stop completely. As a rule, swelling of the face and lips does not require treatment, although antihistamines can be used to relieve symptoms.
Angioneurotic edema, accompanied by laryngeal edema, can be fatal. Swelling of the tongue, vocal folds, or larynx can lead to airway obstruction. If such symptoms appear, appropriate therapy should be started immediately, for example, inject subcutaneously a solution of epinephrine (adrenaline) at a dilution of 1: 1000 (0.3-0.5 ml) and / or ensure airway patency.
A higher risk of angioedema has been reported in black patients.
Patients with a history of angioedema not associated with the use of ACE inhibitors may be at increased risk of its development when taking drugs of this group.
In rare cases, against the background of therapy with ACE inhibitors, angioedema of the intestine develops. At the same time, patients complain of abdominal pain as an isolated symptom or in combination with nausea and vomiting, in some cases without prior angioedema of the face and at a normal level of C1-esterase. Diagnosis was by CT, abdominal ultrasound, or surgery. Symptoms disappear after stopping ACE inhibitors. Therefore, in patients with complaints of pain in the abdominal region, taking ACE inhibitors, when conducting differential diagnosis, it is necessary to take into account the possibility of developing angioedema of the intestine.
MTOR inhibitors
In patients concurrently taking mTOR inhibitors (for example, sirolimus, everolimus, temsirolimus), therapy may be accompanied by an increased risk of angioedema (for example, swelling of the upper airways or tongue with or without respiratory disorders).
Anaphylactoid reactions during desensitization
There are isolated reports of the development of anaphylactoid reactions in patients who took ACE inhibitors during desensitizing therapy (for example, the venom of hymenoptera insects: bees, wasps). ACE inhibitors should be used with caution in patients with a history of allergy or a tendency to allergic reactions during desensitization. The use of an ACE inhibitor should be avoided in patients receiving immunotherapy with hymenoptera venom. The development of such reactions can be avoided by temporarily discontinuing ACE inhibitors at least 24 hours before the start of the desensitization procedure.
Anaphylactoid reactions during LDL apheresis
In rare cases, patients receiving ACE inhibitors have developed life-threatening anaphylactoid reactions during LDL apheresis with dextran sulfate. To prevent such reactions, you should temporarily stop taking ACE inhibitors before each apheresis procedure.
Hemodialysis
Rarely, patients receiving ACE inhibitors have developed anaphylactoid reactions during hemodialysis using high-flow membranes (eg, AN69®). Therefore, it is recommended to use a different type of membrane or to use an antihypertensive drug of another pharmacotherapeutic group.
Primary hyperaldosteronism
Patients with primary hyperaldosteronism, as a rule, are refractory to antihypertensive drugs, the action of which is based on inhibition of the RAAS. Therefore, the use of this drug is not recommended.
Pregnancy
ACE inhibitors should not be started during pregnancy. Those planning a pregnancy should be prescribed an alternative antihypertensive drug with an established safety profile for use during pregnancy. If pregnancy is detected, treatment with ACE inhibitors should be discontinued immediately, and, if necessary, alternative antihypertensive therapy should be prescribed.
Cough
During therapy with ACE inhibitors, a dry persistent cough may occur. The cough persists for a long time while taking drugs of this group and disappears after they are canceled. When a dry cough appears in a patient, one should be aware of the possibility of its appearance in connection with the intake of an ACE inhibitor. If it is necessary to use drugs of this group, the administration of an ACE inhibitor can be continued.
Surgery / general anesthesia
The use of ACE inhibitors in patients undergoing surgery using general anesthesia can lead to a pronounced decrease in blood pressure, especially when using drugs for general anesthesia with antihypertensive effects. It is recommended that you stop taking long-acting ACE inhibitors, including perindopril, 24 hours before surgery.
Aortic and mitral stenosis, GOKMP
ACE inhibitors should be used with caution in patients with left ventricular outflow tract obstruction.
Atherosclerosis
The risk of developing arterial hypotension exists in all patients, but special care should be taken in patients with coronary artery disease and cerebrovascular diseases. In these patients, treatment is started with low doses of Roxatenz-Inda.
Hyperkalemia
While taking ACE inhibitors, hyperkalemia may develop. Risk factors for hyperkalemia are renal failure, old age (over 70 years), diabetes mellitus, some concomitant conditions (dehydration, acute decompensation of CHF, metabolic acidosis), concomitant use of potassium-sparing diuretics (spironolactone, eplerenone, triamterene, amiloride), potassium preparations, potassium substitutes for table salt, as well as other agents that increase the level of potassium in the blood plasma (for example, heparin, trimethoprim or co-trimoxazole (sulfamethoxazole + trimethoprim) and especially antagonists of aldosterone or ARA II, acetylsalicylic acid ≥3 g / day, COX inhibitors 2 and non-selective NSAIDs, immunosuppressants such as cyclosporine or tacrolimus).
The use of potassium preparations, potassium-sparing diuretics, potassium-containing substitutes for table salt can lead to a significant increase in serum potassium, especially in patients with reduced renal function.
Hyperkalemia can lead to serious, sometimes fatal, heart rhythm disturbances. If necessary, the simultaneous use of Roxatenz-Inda with the above means, you should be careful and regularly monitor the potassium content in the blood plasma.
Ethnic differences
Perindopril, like other ACE inhibitors, apparently has a less pronounced antihypertensive effect in patients of the Negroid race than in other races. Perhaps this difference is due to the fact that in patients with arterial hypertension of the Negroid race, low blood plasma renin activity is more often observed.
Rosuvastatin
Influence on the musculoskeletal system
When using rosuvastatin in all doses, but especially in doses exceeding 20 mg / day, the following effects on the musculoskeletal system have been reported: myalgia, myopathy, in rare cases, rhabdomyolysis. There have been very rare cases of rhabdomyolysis with the simultaneous use of HMG-CoA reductase inhibitors and ezetimibe. This combination should be used with caution, since pharmacodynamic interactions cannot be ruled out.
As in the case of other HMG-CoA reductase inhibitors, the frequency of rhabdomyolysis with post-marketing use of rosuvastatin is higher with a dose of 40 mg / day.
Determination of CPK activity
The serum activity of CPK cannot be determined after intense physical exertion and in the presence of other possible reasons for an increase in its activity, this may lead to an incorrect interpretation of the results obtained. If the initial serum CPK activity is significantly exceeded (5 times higher than the upper limit of the norm), a second analysis should be performed after 5-7 days. You can not start therapy if the results of repeated analysis confirm the initial high serum activity of CPK (more than 5-fold excess of the upper limit of the norm).
Interstitial lung disease
With the use of some HMG-CoA reductase inhibitors, especially for a long time, isolated cases of interstitial lung disease have been reported (see section "Side effects"). Symptoms include shortness of breath, unproductive cough, and deterioration in general well-being (weakness, weight loss, and fever).
If interstitial lung disease is suspected, therapy with HMG-CoA reductase inhibitors should be discontinued.
Before starting therapy
Depending on the daily dose, rosuvastatin should be prescribed with caution to patients with existing risk factors for myopathy / rhabdomyolysis, or the use of Roxatenz-Inda is contraindicated.
These factors include:
• impaired renal function,
• hypothyroidism,
• a history of muscle disease (including a family history),
• myotoxic phenomena when taking other inhibitors of HMG-CoA reductase or fibrates in anamnesis,
• excessive alcohol consumption,
• age over 65,
• conditions in which the concentration of rosuvastatin in the blood plasma may increase,
• simultaneous use of fibrates.
In such patients, it is necessary to assess the risk and possible benefits of therapy. Clinical monitoring is also recommended. If the initial serum CPK activity is more than 5 times higher than the upper limit of the norm, therapy cannot be started.
During therapy
The patient should be informed of the need for immediate medical attention in case of sudden onset of muscle pain, muscle weakness or spasms, especially in combination with malaise and fever. In such patients, the serum activity of CPK should be determined. Therapy should be discontinued if the serum CPK activity is significantly increased (more than 5 times the upper limit of normal) or if muscle symptoms are pronounced and cause daily discomfort (even if the serum CPK activity is no more than 5 times higher than the upper limit of the norm). If symptoms disappear and serum CPK activity returns to normal, consideration should be given to resuming the use of rosuvastatin or other HMG-CoA reductase inhibitors in lower doses with close medical supervision. Control of serum CPK activity in the absence of symptoms is inappropriate.
There have been very rare cases of immune-mediated necrotizing myopathy with clinical manifestations in the form of persistent weakness of the proximal muscles and increased serum CPK activity during therapy or upon discontinuation of the use of HMG-CoA reductase inhibitors, including rosuvastatin.
According to clinical studies, there were no signs of an increase in the effect on skeletal muscles when taking rosuvastatin and concomitant therapy. However, an increase in the number of cases of myositis and myopathy was reported in patients taking other inhibitors of HMG-CoA reductase in combination with fibric acid derivatives (for example, gemfibrozil), cyclosporine, nicotinic acid in lipid-lowering doses (more than 1 g / day), antifungal agents - azole derivatives, HIV protease inhibitors and macrolide antibiotics.
When used simultaneously with some inhibitors of HMG-CoA reductase, gemfibrozil increases the risk of myopathy. Thus, the simultaneous use of rosuvastatin and gemfibrozil is not recommended. The benefits of further altering the plasma lipid concentration with the combined use of rosuvastatin with fibrates or nicotinic acid in lipid-lowering doses should be carefully weighed against the possible risk. Rosuvastatin at a dose of 30 mg / day and 40 mg / day is contraindicated for combination therapy with fibrates.
Due to the increased risk of rhabdomyolysis, rosuvastatin should not be used in patients with acute conditions that may lead to myopathy or conditions that predispose to the development of renal failure (for example, sepsis, arterial hypotension, major surgery, trauma, severe metabolic, endocrine and electrolyte disturbances or uncontrolled seizures).
Rosuvastatin should not be used simultaneously or within 7 days after discontinuation of therapy with fusidic acid preparations. If necessary, the simultaneous use should stop taking rosuvastatin for the period of therapy with fusidic acid. There have been reports of rhabdomyolysis (including fatal) in patients receiving fusidic acid concomitantly with a statin. The patient should see a doctor immediately if any symptoms of muscle weakness, tenderness, or pain appear.
Statin therapy can be resumed 7 days after the last dose of fusidic acid.
In exceptional cases, when long-term systemic therapy with fusidic acid is needed, for example, for the treatment of severe infections, the need for the simultaneous use of rosuvastatin and fusidic acid should be considered on a case-by-case basis and carried out under the strict supervision of a physician.
Protease inhibitors
In patients who received rosuvastatin simultaneously with protease inhibitors and ritonavir, there was an increase in systemic exposure of rosuvastatin. The expected benefit from a decrease in lipid concentration when using rosuvastatin in HIV-infected patients receiving protease inhibitors should be taken into account, and the potential increase in the concentration of rosuvastatin in blood plasma at the beginning of therapy and when titrating the dose of rosuvastatin.
The concomitant use of rosuvastatin with protease inhibitors is not recommended until the dose of rosuvastatin is adjusted.
Ethnic differences
In the course of pharmacokinetic studies in representatives of the Mongoloid race, compared with representatives of the Caucasian race, an increase in the plasma concentration of rosuvastatin was noted.
Influence on the ability to drive vehicles and mechanisms
When driving or working with mechanisms, you should take into account the possibility of dizziness during the treatment period.
As a result, the ability to drive vehicles or other mechanisms may be reduced.
Application for impaired renal function
In patients with severe renal impairment (CC <30 ml / min), use is contraindicated.
Application for violations of liver function
Contraindicated in patients with severe hepatic impairment and in patients with active liver disease.
Use in elderly patients
Before starting to take Roxatenz-Inda, it is necessary to assess the functional activity of the kidneys and the potassium content in the blood plasma. At the beginning of therapy, the dose is selected, taking into account the degree of decrease in blood pressure, especially in the case of a decrease in BCC and loss of electrolytes, which avoids a sharp decrease in blood pressure.
Application in children
The use is contraindicated for children and adolescents under the age of 18
Terms of sell
You can buy Roxatenz-Inda without a doctor's prescription.