Jaundice: causes, symptoms and treatment in children and adults
Jaundice is a fairly common disease, especially among residents of warm countries (Africa, Asia), as well as Eastern Europe, living far from the best social environment.
In this article, we will consider what this disease is, the causes of its occurrence, signs and by what means it can be cured.
Reasons for the appearance
The appearance of the disease is associated with an unacceptably large accumulation of bilirubin, associated with incorrect metabolic processes, when the balance between its formation and excretion from the body is disturbed. This substance is brown crystals, which are among the other components of the main components of bile.
There is indirect (unbound) and associated bilirubin. The first is a consequence of the breakdown of hemoglobin, which is released during the destruction of red blood cells. It is a toxic formation, it does not dissolve in water and is not excreted from the body.
The "birthplace" of this specific formation is the spleen and other important systems (bone marrow, lymph nodes), where it binds to blood proteins with albumin, passes into the liver and turns into a direct one.
Bilirubin is considered a poison. If the body's systems function without failures, it is excreted through the rectum during acts of defecation and urination. If insufficient work of bile excretion pathways is detected, then the vast majority of this substance accumulates in the blood, and the residues are excreted through the skin, as a result of which they change color. When the concentration of this substance in the patient exceeds 2.5 −3 mg / dl, yellowness of the mucous membranes and skin integument occurs.
Jaundice may result from:
a) the appearance of various origin tumors in the liver;
b) pathology in the work and structure of the bile ducts;
c) damage by harmful microbes;
d) undesirable postoperative consequences;
e) the use of certain medications.
Attention! Not to be confused with false, or carotene jaundice, caused by the supersaturation of carotene, formed in the body with excessive use of beets, pumpkins, carrots, citrus fruits, as well as with the use of drugs such as acrychin, picric acid, etc. With false jaundice, yellowness does not affect the mucous membranes, only skin changes color.
The disease is difficult enough to detect in a timely manner, since the incubation period (latent course of the disease) of jaundice can last several weeks, and sometimes several months, depending on the time during which the disease lasts. The disease can occur in the following forms: acute, prolonged, or go into the chronic stage.
Provocative factors
The disease can occur in connection with the ingestion of contaminated foods and water, with a blood transfusion, through sexual contact. If you are afraid of contracting viral hepatitis, you need to remember that contacts with the following people at risk should be minimized:
acquaintances, close relatives infected with this virus;
who had intimate contacts with infected people;
those who intend to travel to a country where the disease is widespread;
drug users.
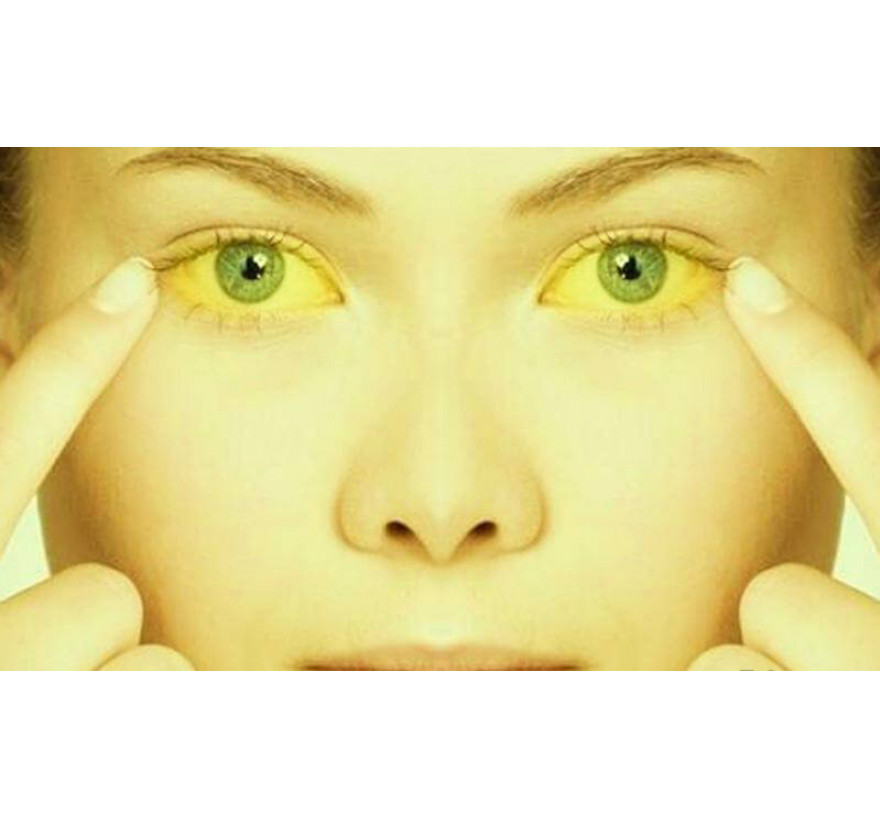
Symptoms of Jaundice
The disease can be detected by the following signs:
yellowness of the skin, eyeballs, sclera;
increased dimensions of the liver and spleen;
high blood red blood cells;
the presence of venous mesh in the abdomen.
In adults, these manifestations are usually accompanied by headache, belching, aversion to food, weight loss, muscle aches, fever, body temperature rises, spasmolytic pain attacks in the right side of the chest, discoloration of feces (excess bilirubin gives them gray color), and urine takes on a dark color.
Types of Jaundice
Not only adults but also children suffer from jaundice. Therefore, we begin with the types of jaundice in children - physiological and neonatal.
Physiological jaundice
Physiological jaundice occurs in babies born (about 60 - 70% of children are affected by it), signs are found on the third or fourth day of life and are caused by adaptation to the new habitat that has arisen. It is recorded in children born before the expiration of the necessary nine-month period, and therefore weakened. The skin, mucous membranes and sclera become yellowish. The baby constantly wants to sleep and does not suck well.
Neonatal jaundice

It can be observed in newborns. It is found in the first two to four days after the birth of the child. It is faced by prematurely appeared babies, twins and those children whose mothers suffer from diabetes.
Jaundice in babies born is not treated with drugs, because it is not, strictly speaking, a disease, the general condition of the body does not cause concern, but is associated with the lack of support for the life support organs, enzyme immaturity, and undeveloped metabolic processes. After a short period of time, it disappears.
If the child’s symptoms do not disappear in the future, it is necessary to resort to treatment. Since indirect bilirubin is a neurotoxic poison, its maximum amount causes severe intoxication of the body, which negatively affects the child’s nervous system, which can subsequently lead to irreversible changes in the cerebral cortex, in the subcortical nuclei and to delay the mental development of the baby.
In adults, other manifestations of this disease are observed.
Conjugation jaundice
It is inherited, it is a non-independent disease (sometimes it can be confused with physiological jaundice), it is detected when there are malfunctions in the course of metabolic processes in the liver, which leads to an increase in the presence of bilirubin in the blood. It appears from the use of certain drugs, as a result of congenital pathologies.
Hemolytic (suprahepatic) jaundice
It is not caused by the pathology of the decay of red blood cells, the high concentration of unnecessary matter and the problems of removing it outside the internal organs. It can be caused by anemia suffered by tropical fever, the result of toxic effects of drugs and if harmful substances such as arsenic, lead, hydrogen sulfide, snake venom get into the body.
Hepatic (parenchymal) jaundice
A very common type of disease. It is associated with a change in the structure and work of hepatocytes. This type is provoked if the patient had cirrhosis of the liver, viral hepatitis, malignant tumors were detected, with drug damage to the liver, excessive consumption of alcohol. The color of the skin changes from yellow to red. Accompanied by the usual manifestations.
Subhepatic (mechanical) jaundice
Its appearance is caused by a violation of the excretion of bile due to narrowing of the gaps of the biliary tract due to the presence of malignant tumors, the existence of helminths, stones in the bile duct, scars, and other reasons. It is characterized by a yellow-green complexion.
Mostly women suffer. In young people, it has a benign character and is a consequence of gallstone disease. In this case, resort to endoscopic papillosphincterotomy (up to 90% of stones in the bile duct are removed). In older women - due to the appearance of a malignant tumor, then radical treatment is necessary.

Diagnostics
If characteristic symptoms occur, you should, without delay, contact a dermatologist, gastroenterologist, hepatologist or infectious disease specialist at the hospital. After an external examination, during which subcutaneous deposits of cholesterol are detected, an increase in the volume and hardness of the liver, spider veins, a decrease in body weight, and conversations about diseases previously suffered by the patient, the doctor prescribes:
analysis of the general and biochemical composition of blood;
tests for the detection of harmful components (including bilirubin) in blood plasma and urine;
ultrasound and tomographic examination of a diseased organ;
sometimes a liver biopsy to determine the nature of the disease and the degree of its development;
Ultrasound and computed tomography of the pancreas and kidneys;
tests for the presence of especially dangerous hepatitis viruses.
After obtaining the results of the tests and establishing the variety of jaundice found in the patient, the doctor prescribes treatment, focusing on the type and stage of the disease.
Treatment
The types of treatment are divided into medical, surgical, the use of physiotherapeutic procedures, the appointment of a diet. For disposable symptoms, conservative treatment is indicated, if the disease is started, resort to surgical intervention (liver transplantation). The goal of treatment is to destroy the remaining bilirubin in the blood plasma, get rid of the virus, prevent the occurrence of cirrhosis and reduce the risk of disease to others.
Conservative therapy
medication: the introduction of antihistamines, corticosteroids. The range of drugs used for treatment is quite wide. Of these, we can mention: Liv 52, Carsil, Ovesol, Essentiale forte. Each has its own specific application.
Important! You can not choose drugs on their own, without consulting a doctor.
physiotherapeutic procedures:
a) the use of plasmapheresis (purification of blood plasma from toxins by filtering it using special apparatuses). This procedure is expensive, especially since several sessions are necessary. They usually spend in medical institutions, sometimes at home. It is indicated in case of liver problems, autoimmune hepatitis, with intoxication of the body;
b) the use of phototherapy;
c) ultrasound in the area of the affected organ;
compliance with the required diet.
If you do not start to be treated in a timely manner, the disease will progress, and perhaps you can not reach the stage of remission. Dangerous complications arise, eliminated only by liver transplantation.
In case of viral hepatitis, antiviral drugs are not used, the drugs used help minimize the concentration of available toxins and remove them from the internal organs.
Patients are given detoxification drugs, glucose, vitamins, and hepatoprotectors, which have a stimulating effect at the cellular level and help restore cell structures. After conducting therapeutic procedures, liver function, as a rule, is fully restored.
Treatment methods vary with different types of disease.
In the case of subhepatic jaundice, an operation is indicated to eliminate the causes that interfere with the excretion of bile masses: remove malignant formations, crush stones, and in some cases remove the gall bladder.
Suprahepatic jaundice - in this case, treat existing anemia. In severe situations, a blood transfusion is necessary.
Infectious jaundice is treated in a hospital. Antiviral therapy is being conducted to help maintain liver function.
Attention! There are no complications of jaundice, since it is a combination of symptoms, but inadequate treatment of jaundice-causing diseases leads to serious damage to body functions.
Diet
To speed up the return to normal life and restore normal metabolism, you must follow an established diet. You should focus on the use of edible products enriched with a complex of vitamins and minerals.
In the acute course of the disease, a carbohydrate diet is prescribed, which includes a large amount of liquid in the form of compotes, jelly, decoctions of vegetables. Steam or boiled fish and meat dishes are introduced into the diet. Oil (vegetable or natural cream) is consumed in limited quantities. For the recovery period, diet No. 5 is used - low-fat dairy products, low-fat meat and fish products, and grain bread. Such a diet can last a whole year.
Since folic acid is needed to restore blood formation methods, it is necessary to include beef and chicken liver, vegetable greens, yeast, cabbage in the diet. To provide the body with fiber, it is proposed to eat oatmeal.
You should limit the use of carrots, citrus fruits, pumpkins. For all types of jaundice, carbonated drinks, strong tea or coffee, chocolate, alcohol, fatty and spicy foods that unnecessarily strain the liver are contraindicated. Fractional nutrition, food is taken in small portions.
Preventive actions
To prevent undesirable consequences, the following conditions must be met:
careful observance of personal hygiene;
do not eat in unsanitary conditions: you can eat only washed or heat-treated food, you must wash your hands before eating;
do not take medicine without first consulting a doctor;
avoid frequent contact with carriers of viral hepatitis;
Do not resort to the services of suspicious dental clinics;
correctly alternate work, sleep and rest;
control your weight, avoid obesity;
exclude accidental sex.
An icteric vaccine does not exist, because we are not dealing with a disease, but with a symptom, a pathological manifestation of a latent disease. Today, vaccines are only given against hepatitis B virus.
In conclusion, it is worth saying that the observance of preventive measures and the timely treatment of a doctor in case of warning signs will significantly reduce the risk of jaundice.
