Respiratory failure. Causes, symptoms, signs, diagnosis and treatment of pathology

For any violations that may cause this condition, the so-called compensatory mechanisms are triggered. They maintain the concentration of oxygen and carbon dioxide in the blood at a level as close to normal as possible. Depletion of these mechanisms leads to symptoms of respiratory failure. As a rule, it occurs if the partial pressure of oxygen in the blood drops below 60 mm Hg, or the partial pressure of carbon dioxide rises above 45 mm Hg. Art.
This disease of the respiratory system can have various causes. Respiratory failure develops not only against the background of lung diseases, but also some other systems (cardiovascular, nervous, etc.). However, a chain of disorders in the body, which is triggered by a lack of oxygen, always leads to similar consequences.
The prevalence of this syndrome in society is almost impossible to assess. This condition can last from a few minutes or hours (acute respiratory failure) to several months or years (chronic respiratory failure). It accompanies almost any respiratory disease and occurs with the same frequency in both men and women. According to some reports, the number of people suffering from chronic respiratory failure and requiring active treatment in Europe is 80-100 people per 100,000 population. Without timely qualified assistance, respiratory failure leads to a rapid depletion of compensatory mechanisms and the death of the patient.
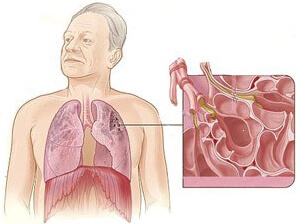
Anatomy and physiology of the lungs
The human respiratory system is a combination of organs and anatomical structures that provide the breathing process. This concept includes not only the act of inspiration and expiration, but also the transfer of oxygen by blood to various organs and tissues, and carbon dioxide to the lungs. This also includes the process of cellular respiration, in which energy is released for the life of the cell. In addition, there are anatomical structures that regulate the work of the respiratory system. They do not directly participate in gas exchange or oxygen transport, but they are related to the normal operation of the system as a whole.
The following departments can be distinguished in the human respiratory system:
upper respiratory tract;
tracheobronchial tree;
respiratory muscles;
respiratory center;
pleural cavity;
blood.
Upper respiratory tract
The upper respiratory tract performs the function of cleaning and warming the air. When passing through them, some of the pathogens are neutralized or delayed. In the development of respiratory failure, this section of the respiratory system plays an indirect role.
The upper respiratory tract includes:
nasal cavity;
oral cavity;
pharynx;
larynx.
Since the airways at this level are quite wide, their blockage is rarely observed. This is possible with the retraction of the root of the tongue, when it overlaps the lumen of the pharynx, swelling of the mucous membrane of the throat. Most often, this can lead to respiratory failure in children. Their edema of the epiglottis quickly blocks the way of the inhaled air.
In addition, a number of changes in the upper respiratory tract may increase the likelihood of certain diseases of the respiratory system. For example, with a stuffy nose, the patient breathes with his mouth. Because of this, the air is worse cleared, moistened and warmed up. Increases the likelihood of contracting bronchitis or pneumonia, which, in turn, will cause respiratory failure.
Tracheobronchial tree
The tracheobronchial tree is a set of airway passages that carry air during inspiration into the lungs. Air flows sequentially from the trachea into the main bronchi, and from there into the bronchi of a smaller caliber. At this level, several mechanisms for the development of respiratory failure can occur at once.
From an anatomical point of view, the lungs are usually divided into the following parts:
trachea (one central tube going from the larynx to the chest cavity);
main bronchi (2 bronchi distributing air into the right and left lungs);
lobes of the lungs (3 lobes in the right lung and 2 in the left);
segments of the lungs (10 segments in the right lung and 8 in the left);
lung tissue (acini).
It is with the anatomy and physiology of the tracheobronchial tree that respiratory failure is most often associated. Here, air during inhalation is distributed into segments, and inside them through the small bronchi and bronchioles goes to the acini. Acinus is a collection of respiratory alveoli. The alveolus is a small cavity with thin walls, shrouded in a dense network of blood capillaries. This is where the actual gas exchange takes place. Through the walls of the alveoli with the help of special enzymes, oxygen is transferred to the blood and carbon dioxide from the blood.
Alveolar cells perform another important function. They secrete the so-called pulmonary surfactant. This substance prevents spontaneous subsidence or adhesion of the walls of the alveoli. From the point of view of physics, it reduces the force of surface tension.
Respiratory muscles
Respiratory muscles are muscle groups in the chest area that are involved in the process of inspiration. Exhalation, in contrast to inspiration, is a passive process and does not require mandatory muscle tension. In the absence of obstruction in the airways after muscle relaxation, the lungs subside themselves, and air leaves the chest cavity.
The two main groups of respiratory muscles are:
Intercostal muscles. Intercostal are called short muscle bundles that are obliquely between adjacent ribs. With their contraction, the ribs rise slightly and take a more horizontal position. As a result, the circumference of the chest and its volume increase. The lung tissue stretches, drawing air through the airways.
Diaphragm. The diaphragm is a flat muscle consisting of several groups of muscle bundles going in different directions. It is located between the chest and abdominal cavity. At rest, the diaphragm has the shape of a dome, which protrudes upward, towards the chest. During inspiration, the dome is flattened, the abdominal organs are shifted slightly down, and the volume of the chest increases. Since the pleural cavity is hermetic, pulmonary tissue is stretched after the diaphragm. There is a breath.
There are additional groups of respiratory muscles, which normally perform other functions (head, upper limb movements, extension of the back). They are included only when the two above groups can not cope with maintaining breathing.
Respiratory Center
The respiratory center is a complex system of nerve cells, the bulk of which is located in the medulla oblongata (brain stem). It is the highest link in the regulation of the breathing process. The cells of the center are automatic. This supports the breathing process during sleep and in an unconscious state.
Actually respiration is regulated by specific receptors. They capture changes in the pH of the blood and cerebrospinal fluid. The fact is that with the accumulation of too high a concentration of carbon dioxide in the blood, the pH drops (acidosis develops). Receptors pick it up and transmit signals to the respiratory center. From there, the nerves go to a team to other organs of the respiratory system (for example, rapid contraction of the respiratory muscles, expansion of the bronchi, etc.). Due to this, ventilation of the lungs is enhanced, and an excess of carbon dioxide is removed from the blood.
Disorders at the level of the respiratory center disrupt the entire system. Even if automatism persists, an adequate reaction of the respiratory system to a decrease in pH may be impaired. This is the cause of severe respiratory failure.
Pleural cavity
The pleural cavity is by and large not a part of the respiratory system. This is a small gap between the wall of the chest and the surface of the lung. However, pathologies in this area often lead to the development of respiratory failure.
The pleura itself is the external serous membrane that covers the lungs and lines the chest cavity from the inside. The sheet of the membrane that covers the lung tissue is called visceral, and the one that lines the walls is called parietal (parietal). These sheets are soldered together, so the space they form is hermetically sealed, and it maintains a pressure slightly below atmospheric.
Pleura performs two main functions:
Excretion of pleural fluid. Pleural fluid is formed by special cells and “lubricates” the inner surfaces of the pleural sheets. Due to this, the friction between the lungs and the walls of the chest during inhalation and exhalation practically disappears.
Participation in the act of breathing. The act of breathing is an expansion of the chest. The lungs themselves do not have muscles, but are elastic, so they expand after the chest. The pleural cavity in this case acts as a pressure buffer. With the expansion of the chest, the pressure in it drops even lower. This leads to stretching of the lung tissue and the entry of air into it.
If there is a violation of the integrity of the pleura, the breathing process is disrupted. The chest is stretched, but the pressure in the pleural cavity does not drop. Air or liquid is drawn in there (depending on the nature of the defect). Since the pressure does not drop, the lung tissue does not stretch and inspiration does not occur. That is, the chest moves, but oxygen does not enter the tissues.
Blood
Blood in the body performs many functions. One of the main is the transportation of oxygen and carbon dioxide. Thus, blood is an important link in the respiratory system, directly connecting the respiratory system with other tissues of the body.
In the blood, oxygen is transported by red blood cells. These are red blood cells containing hemoglobin. Once in the capillary network of the lungs, red blood cells take part in the process of gas exchange with air contained in the alveoli. Direct transfer of gases through the membrane is carried out by a set of special enzymes. On inspiration, hemoglobin binds oxygen atoms, turning into oxyhemoglobin. This substance has a bright red color. After this, red blood cells are transferred to various organs and tissues. There in living cells, oxyhemoglobin gives off oxygen and binds to carbon dioxide. A compound called carboxyhemoglobin is formed. It transports carbon dioxide to the lungs. There, the compound breaks down, and carbon dioxide is released with exhaled air.
Thus, in the development of respiratory failure, blood also plays a role. For example, the number of red blood cells and hemoglobin directly affects how much oxygen can bind a certain amount of blood. This indicator is called the oxygen capacity of the blood. The stronger the level of red blood cells and hemoglobin falls, the faster respiratory failure develops. Blood simply does not have time to deliver the right amount of oxygen to the tissues. There are a number of physiological indicators that reflect the transport functions of the blood. Their definition is important for the diagnosis of respiratory failure.
The following indicators are considered normal:
The partial pressure of oxygen is 80-100 mmHg (mmHg). Reflects blood oxygenation. A drop in this indicator indicates hypoxemic respiratory failure.
The partial pressure of carbon dioxide is 35 - 45 mm Hg. Art. Reflects blood saturation with carbon dioxide. An increase in this indicator indicates hypercapnic respiratory failure. It is important to know the partial pressure of gases for the purpose of oxygen therapy and mechanical ventilation.
The number of red blood cells is 4.0 - 5.1 for men, 3.7 - 4.7 - for women. The rate may vary with age. With a lack of red blood cells, anemia develops, and individual symptoms of respiratory failure appear even during normal lung function.
The amount of hemoglobin is 135 - 160 g / l for men, 120 - 140 g / l for women.
The color indicator of blood is 0.80 - 1.05. This indicator reflects the saturation of red blood cells with hemoglobin (each red blood cell may contain a different amount of hemoglobin). More modern methods use another way to determine this indicator - SIT (the average hemoglobin content in a single red blood cell). The norm is 27 - 31 picograms.
Saturation of blood with oxygen - 95 - 98%. This indicator is determined using pulse oximetry.
With the development of respiratory failure and hypoxia (lack of oxygen), a whole series of changes develop in the body, which are called compensatory mechanisms. Their task is the longest and most complete support of the level of oxygen in the blood at the proper level.
Compensatory mechanisms for hypoxia are:
Tachycardia. Tachycardia or heart palpitations occurs in order to pump blood faster in a small circle of blood circulation. Then its larger volume will have time to be saturated with oxygen.
Increased stroke volume of the heart. In addition to tachycardia, the walls of the heart themselves begin to stretch more, allowing them to pump more blood in one reduction.
Tachypnea. Tachypnea is rapid breathing. It appears in order to pump a larger volume of air. This compensates for the lack of oxygen in cases where a segment or lobe of the lung is not involved in the breathing process.
Inclusion of auxiliary respiratory muscles. The auxiliary muscles, which were already mentioned above, contribute to the rapid and strong expansion of the chest. Thus, the volume of air entering during inspiration increases. All four of the above mechanisms are activated in the first minutes when hypoxia occurs. They are designed to compensate for acute respiratory failure.
An increase in circulating blood volume. Since oxygen is distributed throughout the tissues by the blood, hypoxia can also be compensated by an increase in blood volume. This volume appears from the so-called blood depots, which are the spleen, liver, and capillaries of the skin. Their emptying increases the amount of oxygen that can be transported to the tissues.
Myocardial hypertrophy. The myocardium is the heart muscle that carries out contractions of the heart and pumps blood. Hypertrophy is a thickening of this muscle due to the appearance of new fibers. This allows the myocardium to work in enhanced mode longer, supporting tachycardia and increasing stroke volume. This compensatory mechanism develops over months or years of illness.
Increased red blood cell levels. In addition to increasing the volume of blood, in general, the content of red blood cells in it (erythrocytosis) also increases. With them, the hemoglobin level also increases. Due to this, the same volume of blood is able to bind and transfer a larger volume of oxygen.
Tissue adaptation. The tissues of the body themselves in conditions of lack of oxygen begin to adapt to new conditions. This is expressed in slowing down cellular reactions, slowing down cell division. The goal is to reduce energy costs. Glycolysis (decomposition of accumulated glycogen) is also enhanced to release additional energy. Because of this, patients who suffer from hypoxia for a long time lose weight and gain poor weight, despite good nutrition.
The last four mechanisms appear only some time after the establishment of hypoxia (weeks, months). Therefore, these mechanisms are activated mainly in chronic respiratory failure. It should be noted that in some patients not all compensatory mechanisms may be involved. For example, with pulmonary edema caused by heart problems, there will no longer be tachycardia or increased stroke volume. If the respiratory center is damaged, there will be no tachypnea.
Thus, from the point of view of anatomy and physiology, the breathing process is supported by a very complex system. With various diseases, disorders can occur at its most diverse levels. The result is always respiratory failure with the development of respiratory failure and oxygen starvation of tissues.
Causes of Respiratory Failure
As mentioned above, respiratory failure can have many different causes. Usually these are diseases of various organs or systems of the body that have led to impaired lung function. Respiratory failure can also occur with injuries (head, chest) or in accidents (foreign body stuck in the airways). Each cause leaves a certain imprint on the pathological process. Its definition is very important for an adequate treatment of the problem. Completely eliminate all manifestations of this syndrome can only eliminate its root cause.
Respiratory failure may occur in the following situations:
disorders of the central nervous system (CNS);
damage to the respiratory muscles;
chest deformity;
airway obstruction;
disorders at the level of the alveoli.
Disorders of the central nervous system
As mentioned above, the main link in the regulation of the respiratory process is the respiratory center in the medulla oblongata. Any disease or any pathological condition that disrupts its work leads to the development of respiratory failure. The cells of the respiratory center cease to adequately respond to an increase in the concentration of carbon dioxide in the blood and a drop in the level of oxygen. A peculiar command does not go along the nerves to correct the growing imbalance. As a rule, it is disorders at the central nervous system that lead to the most severe types of respiratory failure. Here will be the highest mortality rate.
The following phenomena can lead to damage to the respiratory center in the medulla oblongata:
Overdose of drugs. A number of narcotic drugs (primarily heroin and other opiates) can directly inhibit the activity of the respiratory center. With an overdose, it can decrease so much that the respiratory rate drops to 4 - 5 breaths per minute (with a norm of 16 - 20 in adults). Of course, under such conditions, the body does not receive enough oxygen. Carbon dioxide is accumulating in the blood, but the respiratory center does not respond to an increase in its concentration.
Head injury. Serious head injuries can lead to direct damage to the respiratory center. For example, with a strong blow to the area below the occipital protuberance, a fracture of the skull occurs with damage to the medulla oblongata. In most cases, serious injuries in this area are fatal. The neural connections in the area of the respiratory center are simply broken. Since nerve tissue regenerates most slowly, the body cannot compensate for such damage. Breathing stops completely. Even if the respiratory center itself is not damaged, brain edema may develop after the injury.
Electrical injury. An electric shock can cause a temporary “shutdown” of the respiratory center and blockage of nerve impulses. In this case, there will be a strong decrease or a complete stop of breathing, which often leads to death. Only a sufficiently strong electric shock (third degree of electrical injury) can lead to such consequences.
Cerebral edema. Cerebral edema is an emergency in which fluid begins to accumulate in the cranium. It compresses nerve tissue, leading to a variety of disorders. The most difficult option is the appearance of so-called stem symptoms. They appear when an increased volume of fluid “pushes” the brain stem into a large occipital foramen. The so-called wedge of the brain stem occurs and its strong compression. This leads to disturbances in the work of the respiratory center and the development of acute respiratory failure. In addition to injuries, increased blood pressure, a violation of the protein composition of the blood, and some infections can lead to cerebral edema. Timely lowering of pressure in the cranial box (medically or surgically) prevents wedging of the brain stem and the appearance of respiratory failure.
Circulatory disturbance in the brain. In some cases, the respiratory center stops working due to acute circulatory arrest. This is due to a stroke. It can be hemorrhagic (with rupture of the vessel) or ischemic (with clogging of the vessel with a blood clot). If the respiratory center also enters the area left without blood supply, its cells die and cease to fulfill their functions. In addition, cerebral hemorrhages (massive hematomas) increase intracranial pressure. It turns out a situation similar to cerebral edema, when the respiratory center is compressed, although there is no direct violation of blood circulation in this zone.
Spinal injury The central nervous system includes not only the brain, but also the spinal cord. Nerve bundles pass through it, which transmit impulses to all organs. Injury to the cervical or thoracic region may damage these bundles. Then the connection between the respiratory center and the underlying departments is broken. As a rule, in these cases the respiratory muscles fail. The brain sends signals with a normal frequency, but they do not reach the destination.
Hypothyroidism Hypothyroidism is called a decrease in the level of thyroid hormones in the blood (thyroxine and triiodothyronine). These substances regulate many different processes in the body. In severe cases, the nervous system is affected. In this case, the bioelectric impulse is transmitted worse through the nerves. The activity of the respiratory center itself may directly decrease. In turn, various thyroid diseases (autoimmune thyroiditis, removal of the thyroid gland without adequate replacement therapy, inflammation of the gland, etc.) lead to hypothyroidism. In medical practice, these causes rarely cause serious respiratory failure. Adequate treatment and normalization of hormone levels quickly eliminates the problem.
The defeat of the respiratory muscles
Sometimes respiratory failure can be caused by problems at the level of the peripheral nervous system and muscle system. As mentioned above, to ensure a normal act of breathing, the human body uses many muscles. With a number of diseases, they can cope poorly with their functions, despite the normal functioning of the respiratory center. An impulse comes to the muscles, but their contraction is not strong enough to overcome the pressure inside the chest and straighten the lungs. This cause of respiratory failure is quite rare in medical practice, but is difficult to treat.
The main causes of respiratory muscle weakness are the following diseases:
Botulism. Botulism is a toxic infection disease that is caused by the ingestion of the so-called botulinum toxin. This substance is one of the strongest poisons in the world. It inhibits the activity of motor nerves at the level of the spinal cord, and also blocks the transmission of a bioelectric impulse from a nerve to a muscle (blockade of acetylcholine receptors). Because of this, the respiratory muscles do not contract, and breathing stops. In this case, we will only talk about acute respiratory failure. A similar mechanism for the development of this syndrome can be observed with some other infectious diseases (tetanus, poliomyelitis).
Guillain-Barré Syndrome. This disease is characterized by inflammation of the spinal, cranial and peripheral nerves with impaired conduction of impulses. The reason is an attack by the body of its own cells due to malfunctions of the immune system. In one of the variants of the course of the disease, respiratory failure gradually develops. This is due to lethargy of the respiratory muscles and a violation of its innervation. Without adequate treatment, respiratory arrest may occur.
Duchenne myodystrophy. This disease is characterized by a gradual death of muscle fibers. The cause is a congenital defect in a gene that encodes a protein in muscle cells. The prognosis for Duchenne myodystrophy is unfavorable. Patients throughout life suffer from respiratory failure caused by weakness of the respiratory muscles. With age, it progresses and leads to the death of the patient in 2 to 3 decades of life.
Myasthenia gravis This disease has an autoimmune nature. The body forms antibodies to its own muscle tissue and the thymus gland. Because of this, with generalized forms, patients have respiratory muscle weakness. With modern methods of treatment, it rarely leads to death, but certain symptoms still appear.
Overdose of muscle relaxants. Muscle relaxants are a group of drugs whose main action is muscle relaxation and lowering their tone. Most often, they are used during surgical operations to facilitate the work of the surgeon. In case of accidental overdose of drugs with muscle relaxant effect, the tone of the respiratory muscles can also decrease. Because of this, a deep breath will be impossible, or breathing will stop altogether. In these cases, acute respiratory failure will always develop.
Often, neuromuscular diseases affecting the respiratory muscles do not themselves lead to respiratory failure, but only create favorable conditions for its development. For example, with Duchenne myodystrophy and myasthenia gravis, the risk of a foreign body entering the respiratory tract is greatly increased. Also, patients often develop pneumonia, bronchitis and other infectious processes in the lungs.
Chest deformity
In some cases, the cause of respiratory failure is a change in the shape of the chest. It may be due to trauma or a congenital malformation. In this case, it is a compression of the lungs or a violation of the integrity of the chest. This prevents the lung tissue from expanding normally while contracting the respiratory muscles. As a result, the maximum amount of air that the patient can inhale is limited. Because of this, respiratory failure develops. Most often, it is chronic and can be corrected with surgical intervention.
The causes of respiratory failure regarding the shape and integrity of the chest include:
Kyphoscoliosis. Kyphoscoliosis is one of the options for curving the spinal column. If the curvature of the spine occurs at chest level, this can affect the breathing process. The ribs at one end are attached to the vertebrae, so severe kyphoscoliosis sometimes changes the shape of the chest. This limits the maximum depth of inspiration or makes it painful. Some patients develop chronic respiratory failure. At the same time, with curvature of the spine, nerve roots can be infringed, which will affect the work of the respiratory muscles.
Pneumothorax. Pneumothorax is the accumulation of air in the pleural cavity. It occurs due to rupture of the lung tissue or (more often) due to a chest injury. Since this cavity is normally airtight, air quickly begins to draw in there. As a result, when you try to inhale, there is an expansion of the chest, but the lung on the affected side does not stretch and does not draw in air. Under the influence of its own elasticity, the lung tissue decreases, and the lung turns off from the breathing process. Acute respiratory failure occurs, which, without qualified assistance, can lead to the death of the patient.
Pleurisy. Pleurisy is a number of diseases of the respiratory system, in which there is inflammation of the pleura. Most often, respiratory failure develops with the so-called exudative pleurisy. In such patients, fluid accumulates between the pleura sheets. It compresses the lung and prevents it from filling with air during inspiration. There is acute respiratory failure. In addition to fluid in the pleural cavity, patients who have had pleurisy may experience another problem with breathing. The fact is that after the inflammatory process subsides, sometimes fibrin “bridges” remain between the parietal and visceral pleura. They also interfere with lung tissue to properly expand on inhalation. In such cases, chronic respiratory failure develops.
Thoracoplasty. This is the name of a surgical operation in which a patient removes several ribs for therapeutic purposes. Previously, this method was quite widely used in the treatment of tuberculosis. Now they resort to it less often. After thoracoplasty, the chest volume may slightly decrease. Her breathing movements also reduce amplitude. All this makes the volume of the deepest breath possible less and can lead to the appearance of symptoms of chronic respiratory failure.
Congenital deformity of the chest. Congenital deformity of the ribs, sternum or thoracic spine can be caused by various reasons. The most common are the baby’s genetic diseases, infections, or certain medications during pregnancy. After birth, the degree of respiratory failure in a child depends on the severity of the malformation. The smaller the volume of the chest, the worse the condition of the patient.
Rickets. Rickets is a childhood illness caused by a lack of vitamin D in the body. Without this substance, bone mineralization is disrupted. They become softer and change shape during the growth of the child. As a result, the chest is often deformed by adolescence. This reduces its volume and can lead to chronic respiratory failure.
Most problems with the shape and integrity of the chest can be resolved surgically (for example, fluid removal and dissection of adhesions in pleurisy). However, in the case of rickets or kyphoscoliosis, possible complications of the operation are sometimes more serious than the problems themselves. In these cases, the feasibility of surgery is discussed individually with the attending physician.

Airway obstruction
Airway obstruction is the most common cause of acute respiratory failure. In this case, we are talking not only about the ingress of a foreign body, but also about diseases in which the airways can overlap at different levels. Most often this happens due to a sharp contraction of smooth muscles or severe swelling of the mucous membrane. If the lumen of the respiratory tract is not completely clogged, then the body can still receive a certain amount of oxygen for some time. Complete blockage leads to asphyxiation (cessation of breathing) and death within 5 to 7 minutes. Thus, acute respiratory failure during airway obstruction poses a direct threat to the patient's life. Assistance should be provided immediately.
The same group includes a number of diseases that pose a slightly lower threat. These are pathologies of the lungs, in which the deformation of the bronchi occurs. In the narrowed and partially overgrown gaps passes only part of the required volume of air. If this problem cannot be resolved surgically, the patient suffers from chronic respiratory failure for a long time.
The causes that cause narrowing or closure of the airway lumen include:
Spasm of the muscles of the larynx. Laryngeal muscle spasm (laryngospasm) is a reflex reaction that occurs in response to some external stimuli. It is observed, for example, with the so-called "dry drowning". A person drowns in water, but the muscles of the larynx contract, blocking access to the trachea. As a result of this, a person suffocates, although water did not enter the lungs. After removing the drowning man from the water, you need to use drugs that relax the muscles (antispasmodics) in order to restore air access to the lungs. A similar protective reaction may occur in response to inhalation of irritating toxic gases. With spasm of the muscles of the larynx, we are talking about acute respiratory failure, which poses a direct threat to life.
Laryngeal edema. Laryngeal edema may be the result of an allergic reaction (Quincke's edema, anaphylactic shock) or the result of pathogenic microorganisms entering the larynx. Under the influence of chemical mediators, the permeability of the vascular walls increases. The liquid part of the blood leaves the vascular bed and accumulates in the mucous membrane. The latter swells, partially or completely blocking the lumen of the larynx. In this case, acute respiratory failure also develops, which threatens the patient's life.
Foreign body contact. Ingestion of a foreign body does not always cause acute respiratory failure. It all depends on at what level the blockage of the air ducts occurred. If the lumen of the larynx or trachea is blocked, then air practically does not enter the lungs. If the foreign body has passed the trachea and stopped in the lumen of a narrower bronchus, then breathing does not stop completely. The patient coughs reflexively, trying to remove the problem. One of the segments of the lungs can subside and turn off from the act of breathing (atelectasis). But other segments will provide gas exchange. Respiratory failure is also considered acute, but does not lead so quickly to death. According to statistics, most often obstruction of the respiratory tract occurs in children (by inhalation of small items) and in adults with food.
Fracture of the cartilage of the larynx. A fracture of the cartilage of the larynx is the result of a strong blow to the throat. Cartilage deformation rarely leads to a complete overlap of the lumen of the larynx (it can be established due to concomitant edema). Often there is a narrowing of the airways. In the future, this problem should be solved surgically, otherwise the patient will suffer from chronic respiratory failure.
Compression of the trachea or bronchi from the outside. Sometimes the narrowing of the lumen of the trachea or bronchi is not directly related to the respiratory system. Some volume formations in the chest can squeeze the airways on the side, reducing their clearance. This variant of respiratory failure develops with sarcoidosis (lymph nodes increase, squeezing the bronchi), mediastinal tumors, large aortic aneurysms. In these cases, to restore respiratory function, it is necessary to eliminate the formation (most often by surgery). Otherwise, it can increase and completely block the lumen of the bronchus.
Cystic fibrosis. Cystic fibrosis is a congenital disease in which too much viscous mucus is secreted into the lumen of the bronchi. It does not clear its throat and, as it accumulates, it becomes a serious obstacle to the passage of air. This disease occurs in children. They suffer from chronic respiratory failure of varying degrees, despite the constant use of drugs that thin the sputum and contribute to its expectoration.
Bronchial asthma. Most often, bronchial asthma is hereditary or allergic in nature. It represents a sharp narrowing of the bronchi of small caliber under the influence of external or internal factors. In severe cases, acute respiratory failure develops, which can lead to the death of the patient. The use of bronchodilators usually relieves the attack and restores normal ventilation of the lungs.
Bronchiectatic pulmonary disease. In bronchiectatic pulmonary disease, respiratory failure develops in the late stages of the disease. First, there is a pathological expansion of the bronchus and the formation of an infectious focus in it. Over time, the chronic inflammatory process leads to the replacement of muscle tissue and wall epithelium with connective tissue (peribronchial sclerosis). At the same time, the bronchus gleam becomes much narrower and the volume of air that can pass through it drops. Because of this, chronic respiratory failure develops. As the narrowing of the new bronchi, the respiratory function decreases. In this case, we are talking about a classic example of chronic respiratory failure, which is difficult for doctors to fight, and which can gradually progress.
Bronchitis. In bronchitis, there is simultaneously increased secretion of mucus and the development of inflammatory edema of the mucous membrane. Most often, this process is temporary. The patient has only some symptoms of respiratory failure. Only severe chronic bronchitis can lead to slowly progressive peribronchial sclerosis. Then chronic respiratory failure will be established.
In general, diseases that cause obstruction, deformation, or narrowing of the airways are some of the most common causes of respiratory failure. If we are talking about a chronic process that requires constant monitoring and taking medication, they talk about chronic obstructive pulmonary disease (COPD). This concept combines a number of diseases in which there is an irreversible narrowing of the airways with a decrease in the volume of incoming air. COPD is the final stage of many lung diseases.
Alveolar disorders
Gas exchange disorders at the alveolar level are a very common cause of respiratory failure. The gas exchange that occurs here can be disrupted due to many different pathological processes. Most often, the alveoli are filled with fluid or they are overgrown with connective tissue. In both cases, gas exchange becomes impossible, and the body suffers from a lack of oxygen. Depending on the specific disease that affects the lung tissue, both acute and chronic respiratory failure can develop.
Diseases that disrupt gas exchange in the alveoli are:
Pneumonia. Pneumonia is the most common disease affecting the alveoli. The main reason for their occurrence is the ingress of pathogens that cause the inflammatory process. The immediate cause of respiratory failure is the accumulation of fluid in the alveolar sacs. This fluid seeps through the walls of the dilated capillaries and accumulates in the affected area. At the same time, during inspiration, air does not enter the departments filled with liquid and gas exchange does not occur. Since part of the lung tissue is turned off from the breathing process, respiratory failure occurs. Its severity directly depends on how extensive the inflammation is.
Pneumosclerosis Pneumosclerosis is the replacement of normal respiratory alveoli with connective tissue. It is formed due to acute or chronic inflammatory processes. Tuberculosis, pneumoconiosis (“dusting” of the lungs with various substances), protracted pneumonia, and many other diseases can result in pneumosclerosis. In this case, we will talk about chronic respiratory failure, and its severity will depend on how large the volume of the lung is sclerosed. There is no effective treatment, as the process is irreversible. Most often, a person suffers from chronic respiratory failure for the rest of his life.
Alveolitis. With alveolitis, we are talking about inflammation of the alveoli. Unlike pneumonia, inflammation here is not the result of infection. It occurs when toxic substances enter, autoimmune diseases or against the background of diseases of other internal organs (liver cirrhosis, hepatitis, etc.). Respiratory failure, as in pneumonia, is caused by swelling of the walls of the alveoli and the filling of their cavity with fluid. Often, alveolitis eventually passes into pneumosclerosis.
Pulmonary edema. Pulmonary edema is an emergency in which a large amount of fluid accumulates rapidly in the alveoli. Most often this is due to a violation of the structure of the membranes that separate the capillary bed from the cavity of the alveoli. Liquid seeps through the barrier membrane in the opposite direction. There may be several reasons for this syndrome. The most common is an increase in pressure in the pulmonary circulation. This occurs with pulmonary embolism, some heart diseases, squeezing of the lymphatic vessels, through which part of the fluid normally flows. In addition, the cause of pulmonary edema may be a violation of the normal protein or cellular composition of the blood (osmotic pressure is violated, and the fluid is not retained in the capillary bed). The lungs fill up quickly so that part of the foaming fluid is released when coughing. Of course, we are no longer talking about any gas exchange. With pulmonary edema, acute respiratory failure always occurs, threatening the patient's life.
Respiratory distress syndrome. With this syndrome, lung damage is complex. Respiratory function is impaired due to inflammation, the release of fluid into the cavity of the alveoli, proliferation (cell proliferation). At the same time, surfactant formation and decay of whole lung segments may be impaired. As a result, acute respiratory failure occurs. It may take several days from the onset of the first symptoms (shortness of breath, shortness of breath) to severe lack of oxygen, but usually the process develops faster. Respiratory distress syndrome occurs when inhaling toxic gases, septic shock (the accumulation of a large number of microbes and their toxins in the blood), acute pancreatitis (due to the entry of pancreatic enzymes into the blood).
Destruction of lung tissue. In some diseases, lung tissue is destroyed with the formation of volume cavities that are not involved in the breathing process. With advanced tuberculosis, for example, melting (caseous necrosis) of the walls of the alveoli occurs. After the infection has subsided, large cavities remain. They are filled with air, but do not participate in the breathing process, as they relate to the "dead space". Also, the destruction of lung tissue can be observed with purulent processes. Under certain conditions, pus can accumulate to form an abscess. Then, even after emptying this cavity, normal alveoli no longer form in it, and it will not be able to take part in the breathing process.
In addition to the above reasons, some diseases of the cardiovascular system can lead to symptoms of respiratory failure. In this case, all respiratory organs will work in normal mode. Blood will be enriched with oxygen, but it will not spread to organs and tissues. In fact, for the body the consequences will be the same as with respiratory failure. A similar picture is observed with diseases of the hematopoietic system (anemia, methemoglobinemia, etc.). Air enters the cavity of the alveoli without problems, but cannot communicate with blood cells.
Types of Respiratory Failure
Respiratory failure is a condition that occurs with a variety of pathological processes and for various reasons. In this regard, to simplify the work of doctors and more effective treatment, a number of classifications have been proposed. They describe the pathological process according to various criteria and help to better understand what is happening to the patient.
Different countries have adopted different classifications of respiratory failure. This is due to a slightly different tactic of assistance. However, in general, the criteria are the same everywhere. The types of the pathological process are determined gradually in the process of diagnosis and are indicated in the formulation of the final diagnosis.
The following classifications of respiratory failure are:
classification according to the speed of development of the process;
classification by the phase of the development of the disease;
severity classification;
gas balance violation classification;
classification by the mechanism of the syndrome.
Speed Classification
This classification is perhaps the basic. She divides all cases of respiratory failure into two large types - acute and chronic. These species are very different from each other both for reasons and symptoms, and for treatment. It is usually easy to distinguish one species from another even during the initial examination of the patient.
The two main types of respiratory failure have the following features:
Acute respiratory failure is characterized by a sudden onset. It can develop within a few days, hours, and sometimes several minutes. This type is almost always a threat to life. In such cases, the body's compensatory systems do not have time to turn on, so patients need urgent intensive care. This type of respiratory failure can be observed with mechanical injuries of the chest, obstruction of the airways by foreign bodies, etc.
For chronic respiratory failure, on the contrary, a slow progressive course is characteristic. It develops over many months or years. As a rule, it can be observed in patients with chronic diseases of the lungs, cardiovascular system, and blood. In contrast to the acute process, the compensatory mechanisms mentioned above are successfully starting to work here. They can reduce the negative effect of a lack of oxygen. If complications arise, treatment is ineffective or the disease progresses, the chronic course can become acute with a threat to life.
Classification by phase of the development of the disease
This classification is sometimes used in the diagnosis of acute respiratory failure. The fact is that in most cases with respiratory failure in the body, a series of sequential changes occurs. They are distinguished in 4 main phases (stages), each of which has its own symptoms and manifestations. A correctly defined phase of the pathological process allows for more effective medical care, therefore this classification has practical application.
The following stages are distinguished in the development of acute respiratory failure:
Initial stage. In the initial stage, there may not be vivid clinical manifestations. The disease is present, but does not make itself felt at rest, since the compensatory mechanisms mentioned above begin to work. At this stage, they make up for the lack of oxygen in the blood. With a little physical exertion, shortness of breath, rapid breathing may appear.
Subcompensated stage. At this stage, the compensatory mechanisms begin to deplete. Dyspnea appears even at rest, and breathing is difficult to recover. The patient assumes a posture involving additional respiratory muscles. During an attack of shortness of breath, the lips may turn blue, dizziness appears, and the heartbeat becomes more frequent.
Decompensated stage. In patients in this phase, the compensatory mechanisms are depleted. Blood oxygen levels are greatly reduced. The patient takes a forced position, when changing which there is a severe attack of shortness of breath. Psychomotor agitation may appear, the skin and mucous membranes have a pronounced blue tint. Blood pressure drops. At this stage, urgent medical care is necessary to maintain breathing through medication and special manipulations. Without such help, the disease quickly passes into the terminal stage.
Terminal stage. In the terminal stage, almost all symptoms of acute respiratory failure are present. The patient's condition is very serious due to a strong decrease in the level of oxygen in arterial blood. There may be a loss of consciousness (up to a coma), a sticky cold sweat, breathing shallow and frequent, the pulse is weak (filiform). Blood pressure decreases to critical values. Due to acute oxygen deficiency, serious disturbances in the functioning of other organs and systems are observed. The most typical are anuria (lack of urination due to cessation of renal filtration) and hypoxemic cerebral edema. It is not always possible to save a patient in this condition, even if all resuscitation measures are carried out.
The above stages are more typical for acute respiratory failure, developing against the background of severe pneumonia or other diseases of the lung tissue. With obstruction (blockage) of the respiratory tract or failure of the respiratory center, the patient does not go through all these stages sequentially. The initial stage is practically absent, and the subcompensated stage is very short. In general, the duration of these phases depends on many factors. In older people, the first stages usually last longer because of the possibility of tissues to do without oxygen longer. In young children, on the contrary, the process develops faster. Eliminating the cause of respiratory failure (for example, eliminating laryngeal edema or removing a foreign body) leads to a gradual restoration of lung function, and the phases change in the opposite direction.
Severity classification
This classification is necessary to assess the severity of the patient's condition. It directly affects the tactics of treatment. Severe patients are prescribed more radical methods, while with mild forms there is no direct threat to life. The classification is based on the degree of saturation of arterial blood with oxygen. This is an objective parameter that really displays the patient’s condition, regardless of the reasons that caused respiratory failure. Pulse oximetry is done to determine this indicator.
According to severity, the following types of respiratory failure are distinguished:
First degree. The partial pressure of oxygen in arterial blood is from 60 to 79 mm RT. Art. According to pulse oximetry, this corresponds to 90 - 94%.
Second degree. The partial pressure of oxygen is from 40 to 59 mm Hg. Art. (75 - 89% of the norm).
Third degree. The partial pressure of oxygen is less than 40 mm Hg. Art. (less than 75%).
Gas Balance Classification
With respiratory failure of any origin, a number of typical pathological changes occur. They are based on a violation of the normal gas content in arterial and venous blood. It is this imbalance that leads to the appearance of the main symptoms and poses a threat to the patient's life.
Respiratory failure can be of two types:
Hypoxemic. This type involves a decrease in the partial pressure of oxygen in the blood. This leads to tissue starvation by the mechanisms described above. Sometimes it is also called respiratory failure of the first type. It develops against the background of severe pneumonia, acute respiratory distress syndrome, pulmonary edema.
Hypercapnic. In hypercapnic respiratory failure (of the second type), the accumulation of carbon dioxide in the blood occupies a leading place in the development of symptoms. However, oxygen levels may even remain normal, but symptoms still begin to appear. This respiratory failure is also called ventilation. The most common causes are airway obstruction, respiratory depression, respiratory muscle weakness.
Classification by the mechanism of the syndrome
This classification is directly related to the causes of respiratory failure. The fact is that for each of the reasons listed above in the corresponding section, the syndrome develops according to its own mechanisms. In this case, treatment should be aimed specifically at the pathological chains of these mechanisms. This classification is of the greatest importance for resuscitators who need urgent care in critical conditions. Therefore, it is used mainly in relation to acute processes.
According to the mechanism of acute respiratory failure, the following types are distinguished:
Central. The name itself suggests that respiratory failure has developed due to disturbances in the work of the respiratory center. In this case, they will fight with a cause that affects the central nervous system (elimination of toxins, restoration of blood circulation, etc.).
Neuromuscular This type combines all the reasons that disrupt the conduction of an impulse along the nerves and its transmission to the respiratory muscles. In this case, artificial lung ventilation is immediately prescribed. The device temporarily replaces the respiratory muscles to give doctors time to fix the problem.
Thoracodiaphragmatic. This type of respiratory failure is associated with structural abnormalities that lead to an increase in the diaphragm or curvature of the chest. For injuries, surgical intervention may be necessary. Mechanical ventilation will be ineffective.
Obstructive. This type occurs for all reasons leading to disruption of airflow through the respiratory tract (swelling of the larynx, ingestion of a foreign body, etc.). A foreign body is urgently removed, or drugs are given to quickly relieve edema.
Restrictive. This type is perhaps the most severe. With it, the lung tissue itself is affected, its extensibility is violated and the exchange of gases is interrupted. It occurs with pulmonary edema, pneumonia, pneumosclerosis. Structural disturbances at this level are very difficult to eliminate. Often, such patients subsequently suffer from chronic respiratory failure all their lives.
Perfusion. Perfusion is called blood circulation in a specific section of the body. In this case, respiratory failure develops due to the fact that blood for some reason does not enter the lungs in the right amount. The cause may be blood loss, thrombosis of blood vessels that go from the heart to the lungs. Oxygen enters the lungs in full, but gas exchange does not occur in all segments.
In all of the above cases, the consequences at the body level are usually similar. Therefore, it is rather difficult to accurately classify the pathogenetic type of respiratory failure by external signs. Most often this is done only in the hospital after all analyzes and examinations have been completed.
Symptoms of Acute Respiratory Failure
Symptoms of acute respiratory failure are characterized by a fairly rapid onset and increase. The pathological process is rapidly progressing. From the onset of the first symptoms to the creation of a direct threat to the life of the patient, it may take from several minutes to several days. In principle, many of the observed symptoms are also characteristic of chronic respiratory failure, but they appear differently. Common to both cases are signs of hypoxemia (low levels of oxygen in the blood). Symptoms of the disease that caused breathing problems will vary.
Possible manifestations of acute respiratory failure are:
rapid breathing;
heart palpitations;
loss of consciousness;
lowering blood pressure;
dyspnea;
paradoxical movements of the chest;
cough;
participation of the auxiliary respiratory muscles;
swelling of veins on the neck;
Fright
blue skin;
chest pain;
respiratory arrest.
Rapid breathing
Increased respiration (tachypnea) is one of the compensatory mechanisms. It appears with damage to the lung tissue, partial blockage or narrowing of the airways, and the exclusion of a segment from the breathing process. In all these cases, the amount of air that enters the lungs when inhaling is reduced. Because of this, the level of carbon dioxide rises in the blood. It is captured by special receptors. In response, the respiratory center begins to send more impulses to the respiratory muscles. This leads to increased breathing and a temporary restoration of normal ventilation.
In acute respiratory failure, the duration of this symptom ranges from several hours to several days (depending on the specific disease). For example, with swelling of the larynx, breathing can become faster only a few minutes (as the swelling increases), after which it will stop completely (when the lumen of the larynx is closed). With pneumonia or exudative pleurisy, breathing becomes faster as fluid accumulates in the alveoli or pleural cavity. This process can take several days.
In some cases, rapid breathing may not be observed. On the contrary, it gradually decreases if the cause is damage to the respiratory center, weakness of the respiratory muscles or a violation of innervation. Then the compensatory mechanism simply does not work.
Heart palpitations
Heart palpitations (tachycardia) may be the result of increased pressure in the pulmonary circulation. Blood lingers in the vessels of the lungs, and in order to push it through, the heart begins to contract more often and more strongly. Other cardiac arrhythmias (bradycardia, arrhythmia) can occur if heart problems are the cause of respiratory failure. Then, patients can also find other signs of cardiac pathology (pain in the heart, etc.).
Loss of consciousness
Loss of consciousness is a consequence of hypoxemia. The lower the oxygen content in the blood, the worse the various organs and systems work. Loss of consciousness occurs with oxygen starvation of the central nervous system. The brain is simply turned off, as it is no longer able to support basic vital functions. If the cause of acute respiratory failure is a temporary phenomenon (for example, a severe attack of bronchial asthma), then consciousness returns itself after restoration of normal breathing (relaxation of the smooth muscles of the bronchi). This usually happens after a few minutes. If the cause is an injury, pulmonary edema, or other problems that cannot disappear so quickly, the patient may die without regaining consciousness. Sometimes there is also the so-called hypercapnic coma. With her, loss of consciousness is caused by an increased content of carbon dioxide in arterial blood.
Lowering blood pressure
High blood pressure (hypertension) in the pulmonary circulation is often combined with low blood pressure (hypotension) - in large. This is due to blood retention in the vessels of the lungs due to slow gas exchange. When measured using a conventional tonometer, a moderate decrease in blood pressure is detected.
Dyspnea
Shortness of breath (dyspnea) is a violation of the rhythm of breathing, in which a person for a long time can not restore its normal frequency. He seems to lose control of his own breathing and is not able to take a deep, full breath. The patient complains of a lack of air. Usually an attack of shortness of breath provokes physical activity or strong emotions.
In acute respiratory failure, dyspnea progresses rapidly, and the normal breathing rhythm may not be restored without medical attention. This symptom can have various mechanisms of occurrence. For example, with irritation of the respiratory center, dyspnea will be associated with nervous regulation, and with heart diseases, with increased pressure in the vessels of the pulmonary circulation.
Paradoxical chest movements
In certain situations, patients with respiratory failure may notice asymmetrical respiratory movements of the chest. For example, one of the lungs may not take part in the breathing process at all or lag behind the other lung. Slightly less often, you can observe a situation when the chest does not rise during inspiration (the amplitude is reduced), and with a deep breath, the stomach is inflated. This type of breathing is called abdominal and also indicates the presence of a certain pathology.
Asymmetric chest movements can be observed in the following cases:
collapse of the lung;
pneumothorax;
massive pleural effusion on one side;
unilateral sclerotic changes (cause chronic respiratory failure).
This symptom is not typical for all diseases that can cause respiratory failure. It is caused by a change in pressure inside the chest cavity, accumulation of fluid in it, and pain. However, when the respiratory center is damaged, for example, the chest rises and falls symmetrically, but the amplitude of movements is reduced. In all cases of acute respiratory failure without timely assistance, respiratory movements disappear altogether.
