What is colitis?
As part of the diagnosis, feces are examined (coprogram, bacterial culture, for helminths and protozoa), irrigoscopy, colonoscopy with a biopsy of the large intestine mucosa. Treatment is prescribed taking into account the etiological form of the disease, including diet, etiotropic (antibacterial, anthelmintic and other therapy), taking enzymes and eubiotics, herbal medicine, physiotherapy and balneotherapy.
General information
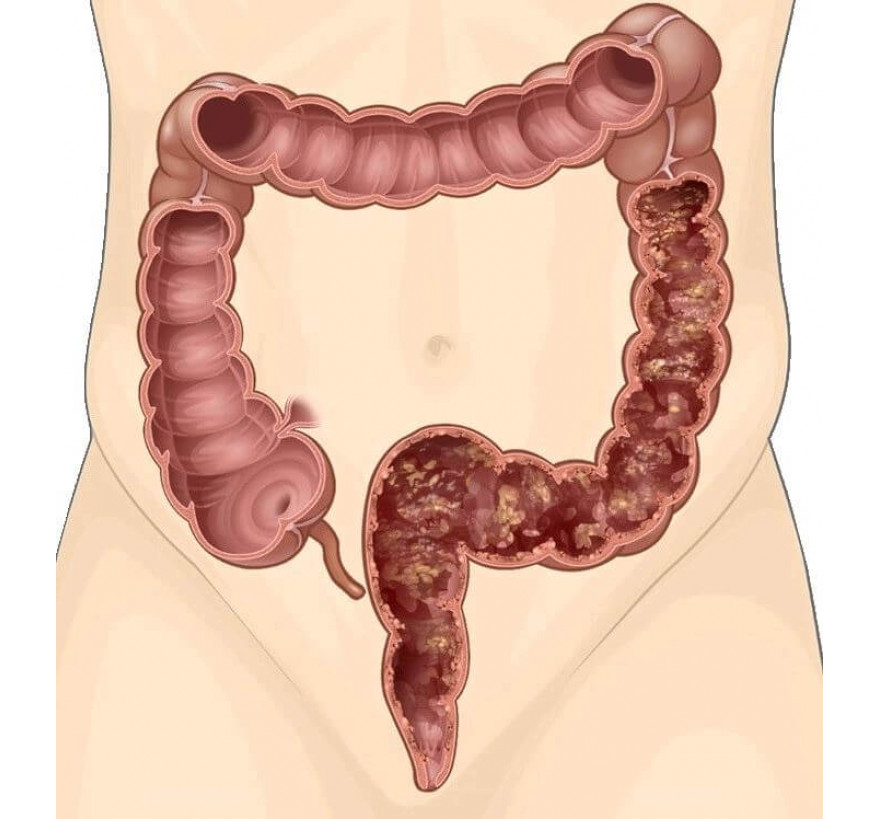
Colitis is a disease of the digestive system, characterized by the development of inflammation in the mucous membrane of the colon wall. There are acute and chronic colitis. Acute colitis is characterized by abdominal pain, flatulence, the presence of mucus and streaks of blood in the feces, nausea, the urge to defecate. A chronic form, ulcerative damage to the intestines, bleeding, and sometimes carcinophobia may develop.
Chronic colitis is a pathological change in the structure of the mucous membrane as a result of a prolonged inflammatory process and dystrophy of the affected tissues, in connection with which there are violations of the motor and secretory function of the large intestine. Chronic colitis is a fairly common disease of the digestive tract, often inflammation of the colon is accompanied by damage to the small intestine.
About a third of patients with chronic colitis note various intestinal infections (most often dysentery and salmonellosis) as the cause of its development. In many cases, the disease develops against the background of dysbiosis (for example, after a long course of antibiotic therapy), due to improper nutrition, a tendency to physical inactivity, and abuse of alcoholic beverages.
Causes of Colitis
The causes of the pathology may be associated with a violation of the regime and nature of the diet (improper eating habits, irregular poor nutrition, alcohol abuse, poor-quality food intake). Colitis can occur as a complication of diseases of the gastrointestinal tract (chronic gastritis, pancreatitis, hepatitis), as well as food poisoning and intestinal infections.
Taking many drugs can have a negative effect on the intestinal flora, iatrogenic dysbiosis can in turn cause inflammatory processes in the large intestine. In addition, drugs that disrupt the acid-base balance in the intestinal lumen can contribute to colitis. Sometimes the causes of inflammatory bowel diseases are congenital developmental pathologies and functional impairment.
Classification
Colitis is divided into infectious (colitis with shigellosis, salmonellosis, mycobacteriosis, tuberculous colitis, etc.), nutritional (associated with malnutrition), toxic exogenous (with prolonged intoxication with mercury vapor, phosphorus, arsenic compounds, etc.) and endogenous (with intoxication with catabolism products, for example, urates with gout), medicinal (developed after the use of drugs: laxatives, aminoglycosides, antibiotics).
Allergic (allergic reaction to food components, drugs, some bacteria or their metabolic products) and mechanical (for chronic constipation, abuse of enemas, rectal suppositories as a result of regular mechanical irritation of the mucosa) colitis are also distinguished. Often there are several etiological factors that contribute to the development of inflammation in the large intestine, then we can talk about combined colitis.
Symptoms of Colitis
For chronic inflammation, such clinical manifestations as abdominal pain, defecation disorder, tenesmus are characteristic. Pain with colitis is characterized by dull aching pain in the lower and lateral parts of the abdomen (often on the left side), or the patient cannot clearly localize the source of the pain (diffuse abdominal pain). After eating, usually the pain intensifies and subsides after bowel movements and gas discharge. In addition, walking, shaking, and a cleansing enema can provoke increased pain. A feeling of heaviness in the abdomen, bloating, flatulence can also be noted.
Stool disorders most often occur in the form of constipation, but an alternation of constipation and diarrhea can be noted. For chronic colitis, diarrhea is characteristic with the release of watery feces with streaks of mucus (sometimes blood may be noted). Tenesmus can occur - false urge to defecate. Sometimes the urge to defecate ends with the release of mucus. In the acute inflammatory process, all of the above symptoms are more pronounced, diarrhea prevails over constipation.
Inflammation of the large intestine most often develops in its terminal sections (proctitis and proctosigmoiditis). Often the cause of colitis in such cases is acute intestinal infection (dysentery) or chronic constipation. In addition, proctosigmoiditis is a frequent result of abuse of cleansing and therapeutic enemas, taking laxatives.
With this form of colitis, the pain is localized from the left iliac region, frequent and painful tenesmus occurs, especially at night. The stool, as a rule, is sparse, it can be like sheep feces, contain large amounts of mucus, less often blood and pus. On palpation of the abdomen, soreness in the projection area of the sigmoid colon is noted. Sometimes a congenital malformation is palpated - an additional sigma loop.
Diagnostics
The complex of obligatory diagnostic measures for suspected colitis includes macro- and microscopy of feces, coprogram, detection of helminth eggs, feces sowing. A general blood test is performed to determine if there are signs of inflammation.
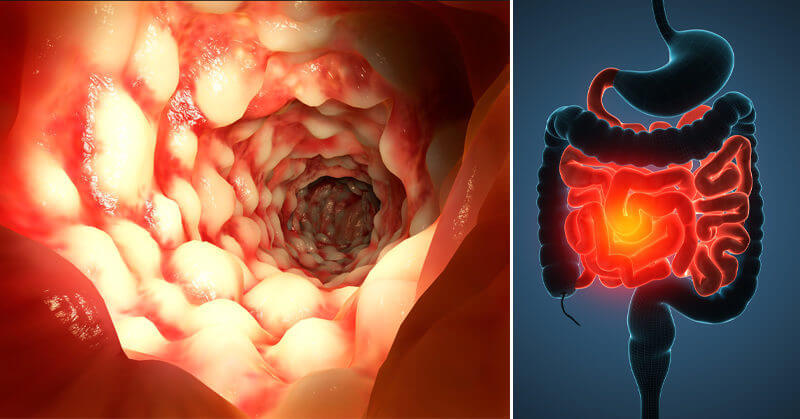
The anatomical and functional features of the large intestine are visualized with contrast irrigoscopy. Colonoscopy allows you to thoroughly examine the condition of the mucosa throughout the colon. In addition, colonoscopy allows you to take biopsies of the intestinal mucosa for further histological examination. To exclude hemorrhoids, anal fissure, paraproctitis and other pathologies, a proctologist examination with a finger study of the anus is indicated.
Differential diagnosis of chronic colitis is performed with dyskinesia of the large intestine. However, it must be remembered that a long-standing disorder of intestinal motility can be complicated by the inflammatory process. Quite often, the clinical picture of colitis can accompany a developing tumor of the large intestine. To exclude malignant tumors, a biopsy of all suspicious sections of the intestinal wall is performed.
In addition, differentiate colitis and enteritis. Sometimes there is inflammation of both sections of the intestine. Data for the differential diagnosis of chronic colitis and diseases of the upper digestive tract give endoscopic studies (colonoscopy, fibrogastroduodenoscopy), ultrasound of the abdominal cavity and functional tests to identify markers of inflammation of the liver and pancreas.
Complications
Colitis can lead to perforation of the intestinal wall with the development of peritonitis (a characteristic complication of severe non-specific ulcerative colitis), intestinal bleeding, which contributes to the development of anemia, intestinal obstruction due to the formation of adhesions, strictures, scars.
Colitis treatment
It is advisable to treat chronic colitis during an exacerbation in a hospital, in the proctology department. Infectious colitis is treated in specialized infectious diseases units. A significant element in the treatment of chronic colitis is the adherence to a therapeutic diet. At the same time, all products that can mechanically or chemically irritate the intestinal mucosa are excluded from the diet, food is consumed in a pureed form, with a frequency of at least 4-5 times a day. In addition, to exclude lactic acid fermentation, patients are advised to abandon milk, in order to reduce gas formation, cabbage and legumes are limited.
From bakery products, dried wheat unsweetened bread is allowed. It is advisable to eat steamed meat and fish of low-fat varieties. When the severe clinical symptoms subside, the diet is gradually expanded. To combat constipation, it is recommended that boiled vegetables, fruit puree (jelly), and bran bread be included in the diet. Improving the passage of intestinal mass contributes to vegetable oil and a sufficient amount of fluid consumed per day. To eat fruits and vegetables raw in the acute period of the disease is undesirable. It is also worth abandoning chilled foods, lactic acid foods and foods high in acid. To regulate the secretion of fluid in the intestine, the use of salt is limited.
In the case of the infectious nature of colitis and to suppress the pathogenic bacterial flora that developed as a result of dysbiosis, antibiotic therapy is prescribed in short courses (ciprofloxacin, Nifuroxazide, rifaximin). Prescribing drugs is done only by a specialist. Identification of eggs of worms is an indication for the appointment of anthelmintic agents. To relieve pain, prescribe antispasmodics (drotaverine, papaverine).
In the treatment of proctosigmoiditis, local therapy is useful: microclysters with decoctions of chamomile, calendula, tannin or protargol. With proctitis, rectal suppositories with belladonna, anesthesin are prescribed to relieve severe pain, astringents (zinc oxide, xeroform). With diarrhea, astringents and enveloping agents are prescribed inside (tannin + albumin, bismuth nitrate, white clay, decoction of oak bark, other decoctions and infusions of collections containing tannic components). With constipation, hydrocolonotherapy is indicated. Severe spasms with colitis can be an indication for the appointment of anticholinergics.
In addition to the above funds, for colitis, enterosorbents can be prescribed (to combat flatulence), enzyme preparations (for digestive disorders due to enzymatic deficiencies), eubiotics (for the correction of dysbiosis). A good effect in the treatment of chronic colitis gives a regular spa treatment, balneotherapy.
Forecast and Prevention
The complex of preventive measures to prevent colitis includes a balanced rational diet, timely detection and treatment of diseases of the digestive system, sanitary-hygienic regimen and compliance with safety regulations in industries associated with hazardous chemical poisons.
Prevention of exacerbations in people suffering from chronic diseases of the large intestine, in addition, include regular follow-up observation by a specialist in the field of clinical proctology. The working capacity of patients with this pathology is limited, they should avoid excessive physical exertion, psycho-emotional stress and activities associated with frequent business trips and contributing to a violation of diet. The prognosis for the timely detection and compliance with medical recommendations for the treatment of chronic colitis is favorable.
