Diphtheria - symptoms and treatment

Definition of the disease. Causes of the disease
Diphtheria (from the Latin diftera - film; pre-revolutionary - “mother’s crying disease”, “mother’s horror disease”) - an acute infectious disease caused by toxigenic strains of diphtheria bacillus, which toxicly affect the circulatory system, nerve tissue and adrenal glands, and also cause fibrinous inflammation in areas of the entrance gate (places of infection). It is clinically characterized by general infectious intoxication syndrome, maxillofacial lymphadenitis, tonsillitis, and local inflammatory processes of a fibrinous nature.
Etiology
Kingdom - Bacteria
genus - Corynebacterium
view - Corynebacterium diphteriae
These are gram-negative sticks located at an angle of V or W. At the ends there are club-shaped bulges (from the Greek coryne - club) due to volutin granules. There is a property of metachromasia - staining is not the color of the dye (according to Neusser - in dark blue, and bacterial cells - in light brown).
Contains lipopolysaccharide, proteins and lipids. In the cell wall there is a cord factor, which is responsible for adhesion (adhesion) to the cells. Colonies of mitis, intermedius, gravis are known. They remain viable in the external environment: under normal conditions they stay alive in air for up to 15 days, in milk and water they survive for up to 20 days, on the surfaces of things - up to 6 months. They lose their properties and die during boiling for 1 minute, in 10% hydrogen peroxide in 3 minutes. Sensitive to disinfectants and antibiotics (penicillins, aminopenicillins, cephalosporins). They love culture media containing sugar (McLaud's chocolate medium).
It isolates pathogenic products such as:
1) Exotoxin (toxin synthesis is determined by the tox + gene, which is sometimes lost), which includes several components:
necrotoxin (causes epithelial necrosis at the entrance gate, damages blood vessels; this leads to plasma exudation and the formation of fibrinoid films, since the enzyme thrombokinase is released from the cells, which converts fibrinogen to fibrin);
true diphtheria toxin is exotoxin (similar in action to cytochrome B, an enzyme of cellular respiration; it replaces cytochrome B in cells and blocks cellular respiration). It has two parts: A (an enzyme that causes a cytotoxic effect) and B (a receptor that promotes the penetration of A into the cell);
hyaluronidase (destroys hyaluronic acid, which is part of the connective tissue, which causes an increase in membrane permeability and the spread of toxin beyond the focus);
hemolyzing factor;
2) Neuraminidase;
3) Cystinase (allows you to distinguish diphtheria bacteria from other types of corynebacteria and diphtheroids). [2] [6]
Epidemiology
Anthroponosis. An infection generator is a person with various forms of diphtheria and a healthy carrier of toxigenic strains of diphtheria microbes. A possible source of infection for humans is domestic animals (horses, cows, sheep), in which the pathogen can be localized on the mucous membranes, cause ulcers on the udder, mastitis.
The most dangerous in terms of the spread of infection are people with diphtheria of the nose, throat and larynx.
Transmission mechanisms: airborne (aerosol), contact (through hands, objects), alimentary route (through milk).
A person is sick who does not have natural resistance (resistance) to the pathogen and does not have the antitoxic immunity of the required level (0.03 - 0.09 IU / ml - conditionally protected, 0.1 and above IU / ml - protected). After a disease, immunity lasts about 10 years, then a second disease is possible. The incidence is affected by the coverage of preventive vaccinations. Seasonality is autumn-winter. During the full course of immunization against diphtheria in childhood and regular revaccination (every 10 years), a strong and stable immunity is developed and maintained, which protects against the disease.
Despite the successes of modern healthcare, mortality from diphtheria at the world level (mainly underdeveloped countries) remains within 10%. [1] [5]
Diphtheria symptoms
The incubation period is from 2 to 10 days.
The course of the disease is subacute (i.e., the main syndrome appears 2-3 days after the onset of the disease), however, with the development of the disease at a young and mature age, as well as with concomitant pathologies of the immune system, it can change.
Diphtheria Syndromes:
general infectious intoxication syndrome;
tonsillitis (fibrinous) - the lead;
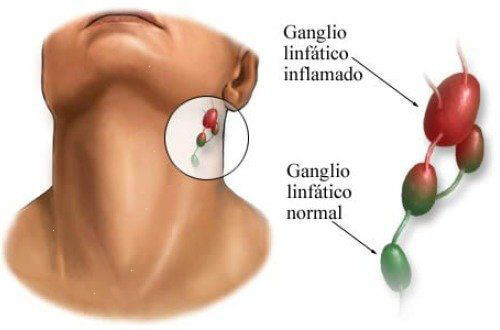
regional lymphadenitis (maxillofacial);
hemorrhagic;
edema of subcutaneous fat.
The onset of the disease is usually accompanied by a moderate rise in body temperature, a general malaise, then the clinical picture diverges according to the form of the disease.
Atypical form (characterized by a short fever for two days, slight discomfort and pain in the throat during swallowing, an increase in the maxillary lymph nodes up to 1 cm, weakly sensitive with light touch);
A typical form (a rather noticeable heaviness in the head, drowsiness, lethargy, weakness, pallor of the skin, an increase in the maxillary lymph nodes from 2 cm or more, pain when swallowing):
a) common (primarily common or developing from localized) - an increase in body temperature to febrile numbers (38-39 ° C), markedly expressed weakness, adynamia, pale skin, drying out in the mouth, sore throat when swallowing moderate intensity, painful lymph nodes up to 3 cm;
b) toxic (primarily toxic or arising from a common one) - severe headache, apathy, lethargy, pallor of the skin, dry mucous membrane of the mouth, possible occurrence of pain in the abdomen in children, vomiting, temperature 39-41 ° C, painful sensations are characteristic throat when swallowing, painful lymph nodes up to 4 cm, edema of subcutaneous fatty tissue around them, extending in some cases to other parts of the body, difficulty in nasal breathing - nasal voice.
The degree of edema of subcutaneous fat:
subtoxic form (edema of the unilateral or parotid region);
toxic I degree (to the middle of the neck);
toxic II degree (to the clavicle);
toxic III degree (edema passes to the chest).
In severe toxic forms of diphtheria due to edema, the neck visually becomes short and thick, the skin resembles a gelatinous consistency (a symptom of "Roman consuls").
Pale skin is proportional to the degree of intoxication. Tonsil attacks are asymmetric.
c) hypertoxic - an acute onset, a pronounced syndrome of general infectious intoxication, obvious changes in the place of the entrance gate, hyperthermia from 40 ° C; acute cardiovascular failure, unstable blood pressure joins;
d) hemorrhagic - impregnation of fibrinous deposits with blood, bleeding from the nasal passages, petechiae on the skin and mucous membranes (red or purple spots that form when capillaries are damaged).
If, in the absence of adequate treatment, body temperature normalizes, then this can not be unequivocally regarded as an improvement - often this is an extremely unfavorable sign.
There are rare diphtheria in vaccinated (similar to atypical diphtheria) and diphtheria in combination with streptococcal infection (there are no fundamental differences).
Other forms of diphtheria infection:
larynx (subfebrile condition - a slight increase in temperature; not pronounced syndrome of general infectious intoxication, at first the catarrhal period - a silent cough with sputum, with difficulty in inhaling (stronger) and exhaling (less pronounced), changes in timbre or loss of voice; then the stenotic period accompanied by difficulties in breathing and retraction of the labile places of the chest; then the period of asphyxia is an excited state, accompanied by sweating, blue skin and subsequently alternating depression eating breathing, drowsiness, cardiac arrhythmias - may result in death);
nose (the temperature is normal or slightly elevated, there is no intoxication, first one nasal passage is affected with the manifestation of a serous-purulent or purulent discharge in it with hemorrhagic impregnation, then the second move. On the wings of the nose there is wetting and crusting, possibly appearing drying crusts on the forehead, cheeks and chin area. Possible edema of the subcutaneous fatty tissue of the cheeks and neck in toxic forms);
eyes (expressed by edema and hyperemia of the conjunctiva of moderate intensity, grayish purulent discharge from the conjunctival sac of moderate severity. In the film form - significant edema of the eyelids and the formation of gray-white films with difficulty on the conjunctiva);
wounds (long-term non-healing wounds with hyperemia of the edges, a dirty gray coating, infiltration of surrounding tissues).
Features with pharyngoscopy:
a) atypical (hyperemia and hypertrophy of palatine tonsils);
b) typical (not pronounced redness with a bluish tint, film plaque, tonsil edema. At the beginning of the disease it is white, then gray or yellow-gray; removed with pressure, tears - leaves a bleeding wound after removal. The film is dense, insoluble and quickly drowns in water, protrudes above the tissue. It is characterized by low pain, as there is anesthesia):
widespread (congestion of congestive-cyanotic color, swelling of the tonsils, soft formations of the oropharynx, film plaque, continuing outside the tonsils);
toxic (the same symptoms as in the common form + tonsils completely block the pharynx, a rough film coating that spreads to the surrounding tissues. Edema of the soft palate. Sometimes a brownish coating - blood impregnation, asymmetry).
Diphtheria pathogenesis
Entrance gates - any areas of the integument (usually the mucous membrane of the oropharynx and larynx). Following the fixation of the bacteria, reproduction occurs at the site of introduction. Further, exotoxin production causes epithelial necrosis, tissue anesthesia, slowing blood flow, the formation of fibrinous films. Diphtheria microbes do not spread beyond the focus, but the toxin spreads through the connective tissue and causes a violation of the functions of various organs:
cardiomyocytes (necrosis - myolysis - infectious toxic myocarditis);
paresis of capillaries (circulatory disorders - toxic toxic shock);
thrombocytopenia, decreased coagulation factors, activation of the fibrinolysis system - hemorrhagic syndrome;
nerve tissue (dystrophy of Schwann cells, demyelination of nerve fibers, primarily regional in relation to the focus - damage to the cranial nerves - paresis and paralysis in 3-5 days. Heart block AV - 90% mortality from diphtheria).
Classification and stages of development of diphtheria
1. In clinical form:
a) atypical (catarrhal);
b) typical (with films):
localized
common;
toxic
2. By severity:
light
average;
heavy.
3. Carrier:
transient (once detected);
short-term (up to 2 weeks);
average duration (15 days - 1 month);
protracted (up to 6 months);
chronic (more than 6 months).
4. By localization:
pharynx (90% occurrence);
larynx (localized and widespread);
nose, eyes, genitals, skin, wounds, combined.
5. With diphtheria of the pharynx:
a) atypical;
b) typical:
localized (insular and membranous);
common;
toxic: subtoxic, toxic I degree, toxic II degree, toxic III degree, hypertoxic, hemorrhagic [3] [8] (with diphtheria of the larynx there is no toxic form, since there is no connective tissue).
Diphtheria Complications
1-2 weeks: infectious toxic myocarditis (cardialgia, tachycardia, pallor, sprawling heart borders, shortness of breath);
2 weeks: infectious toxic polyneuropathy (III, VI, VII, IX, X);
4-6 weeks: paralysis and paresis (flaccid peripheral - paresis of the soft palate);
infectious toxic shock;
infectious toxic necrosis;
acute adrenal insufficiency (pain in the epigastrium, sometimes vomiting, acrocyanosis, sweating, decreased blood pressure, anuria);
acute respiratory failure (diphtheria of the larynx).
Diagnosis of diphtheria
complete clinical blood test (neutrophilic leukocytosis with a shift to the left, increased ESR);
general clinical analysis of urine (microhematuria, cylindruria, proteinuria);
biochemical blood tests (increased AST in myocarditis);
serological methods (determination of class M and G antibodies by ELISA in blood serum, pathogen nucleic acids by PCR, determination of diphtheria antitoxin by ELISA - it is believed that a titer of 0.01 IU and above is considered reliable protection against diphtheria);
bacteriological method (inoculation of material from the pharynx and nasopharynx onto plates with nutrient medium - preliminary response after 48 hours).
Diphtheria treatment
It is carried out in stationary conditions (mild forms may be unrecognized and treated at home).
The most effective start of therapy in the first three days of the disease. The in-patient mode is box, bed (as there is a risk of heart paralysis). Dates for localized diphtheria - 10 days, for toxic - 30 days, with other forms - 15 days.
Diet number 2 according to Pevzner at the height of the disease (mechanically and chemically sparing, full composition), then diet number 15 (general table).
In the very first time, the administration of anti-diphtheria serum (i / m or iv) after a test is indicated medically:
unburdened course - 15-150 thousand IU;
at risk of adverse outcome - 150-500 thousand IU.
An integral part of treatment is antibiotic therapy (antibiotics of the penicillin, aminopenicillin, cephalosporin series).
Pathogenetic therapy includes detoxification, hormonal support, if necessary.
As symptomatic therapy, drugs of the following groups can be used:
antipyretic at temperatures in adults over 39.5 ℃, in children over 38.5 ℃ (paracetamol, ibuprofen);
local anti-inflammatory and antimicrobial agents (tablets, lozenges, etc.);
sedatives;
antiallergic drugs;
antispasmodics.
Treatment of carriers is carried out using antibiotics for common reasons.
Rules for discharge of patients:
the disappearance of the clinical picture of the disease;
cessation of pathogen excretion (two negative inoculations of mucus from the oropharynx and nose, performed no earlier than 14 days after the clinic normalizes with an interval of 2-3 days).
After discharge from the hospital, final disinfection is carried out in the box.
Forecast. Prevention
The most important way to prevent diseases of severe forms of diphtheria infection worldwide is through vaccination. The primary course is carried out in childhood, then regular revaccinations in the adult state are carried out (once every 10 years). Vaccination does not save from bacterial carriage, but from the toxin produced by the bacterium, which causes a difficult clinical picture. In this light, it becomes clear the need to constantly maintain a protective level of antitoxic immunity, to regularly revaccinate (in the Russian Federation - with the ADS-m vaccine).
